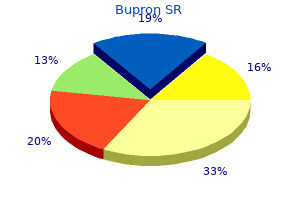
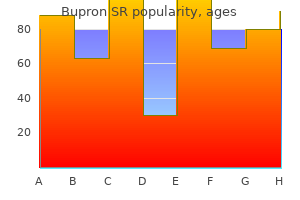
Bupron SR
"Order bupron sr now, mood disorder treatment center".
By: O. Dimitar, M.B.A., M.B.B.S., M.H.S.
Clinical Director, University of Connecticut School of Medicine
Improved stone comminution and simultaneously reduced tissue injury with an upgraded electrohydraulic lithotripter: in vivo studies mood disorder group new york proven bupron sr 150mg. A suppressor to prevent direct wave-induced cavitation in shock wave therapy devices mood disorder 8 year old bupron sr 150 mg low cost. A new transportable shockwave lithotripsy machine for managing urinary stones: a singlecentre experience with a dual-focus lithotripter. Evaluation of synchronous twin pulse technique for shock wave lithotripsy: determination of optimal parameters for in vitro stone fragmentation. Evaluation of synchronous twin pulse technique for shock wave lithotripsy: in vivo tissue effects. Evaluation of a synchronous twinpulse technique for shock wave lithotripsy: the first prospective clinical study. Shock wave lithotripsy at 60 or 120 shocks per minute: a randomized, double-blind trial. Does a slower treatment rate impact the efficacy of extracorporeal shock wave lithotripsy for solitary kidney or ureteral stones The effect of treatment strategy on stone comminution efficiency in shock wave lithotripsy. Progressive increase of lithotripter output produces better in-vivo stone comminution. Effect of escalating versus fixed voltage treatment on stone comminution and renal injury during extracorporeal shock wave lithotripsy: a prospective randomized trial. Prevention of lithotripsy-induced renal injury by pretreating kidneys with low-energy shock waves. Role of adjunctive medical therapy with nifedipine and deflazacort after extracorporeal shock wave lithotripsy of ureteral stones. Is there an adjunctive role of tamsulosin to extracorporeal shockwave lithotripsy for upper ureteric stones: results of an open label randomized nonplacebo controlled study. Effect of alkaline citrate therapy on clearance of residual renal stone fragments after extracorporeal shock wave lithotripsy in sterile calcium and infection nephrolithiasis patients. Citrate and vitamin E blunt the shock wave-induced free radical surge in an in vitro cell culture model. Treatment of renal calculi by lithotripsy: minimizing short-term shock wave induced renal damage by using antioxidants. Stone attenuation and skin-to-stone distance on computed tomography predicts for stone fragmentation by shock wave lithotripsy. The role of mannitol in alleviating renal injury during extracorporeal shock wave lithotripsy. Preminger Introduction to intracorporeal techniques of stone fragmentation the surgical management of nephrolithiasis has undergone dramatic changes over the last 40 years. Developments in radiographic equipment, endourologic devices, and intracorporeal lithotrites have completely changed patient care, thereby providing more effective stone comminution with a significant reduction in operative morbidity compared to the open alternatives. The use of intracorporeal lithotripsy for the management of larger ureteral and intrarenal calculi has dramatically improved. The small working channel of the semi-rigid and flexible endoscopes has limited the size and usefulness of instruments which can be passed and used for stone removal. Indeed, for larger stones, baskets or grasping forceps are often inadequate and potentially dangerous to accomplish successful stone extraction. Although the choice of intracorporeal fragmentation is frequently based on the location and composition of the stone to be treated, the experience of the clinician and availability of equipment often dictates this decision. The intense heat production in the immediate area surrounding the tip of the probe results in a cavitation bubble, which produces a shock wave that radiates spherically in all directions. All particles need to be washed out during intraoperative irrigation, or grasped with forceps. When the vibrating tip is brought in contact with the surface of a stone, the stone can be disintegrated.
The treatment of choice here would be reimplantation of the ureter into the bladder mood disorder rating scale generic bupron sr 150 mg amex. Single-incision minislings versus standard midurethral slings in surgical management of female stress urinary incontinence: a meta-analysis of effectiveness and complications walking depression definition bupron sr 150 mg online. Guimaraes M, Oliveira R, Pinto R, Soares A, Maia E, Botelho F, Sousa T, Pina F, Dinis P, Cruz F. Intermediate-term results, up to 4 years, of a bone-anchored male perineal sling for treating male stress urinary incontinence after prostate surgery. Updated systematic review and meta-analysis of the comparative data on colposuspensions, pubovaginal slings, and midurethral tapes in the surgical treatment of female stress urinary incontinence. Can we, and do we need to , define bladder neck hypermobility and intrinsic sphincteric deficiency Overflow incontinence this occurs when a patient develops chronic urinary retention due to incomplete bladder emptying. This is most commonly seen in elderly men with an enlarged obstructive prostate, however younger men with urethral strictures may also develop this. The bladder distends with chronic retention due to incomplete emptying and this may cause back pressure on the ureters and kidneys affecting renal function. Three surgical procedures for genuine stress incontinence: five-year follow-up of a prospective randomized study. Tension-free vaginal tape versus colposuspension for primary urodynamic stress incontinence: 5-year follow up. Long-term results of artificial urinary sphincter for women with type iii stress urinary incontinence. Urinary symptoms and incontinence in women: relationships between occurrence, age, and perceived impact. Prevalence of urinary incontinence and associated risk factors in postmenopausal women. Urodynamic appraisal of the Bonney test in women with stress urinary incontinence. Prolapse can involve the anterior, middle (apical), or posterior compartment, or a combination of all of them. The posterior compartment represents the rectum (rectocoele), which can also involve the small bowel (rectoenterocoele). The goal of reconstructive surgery is to restore normal vaginal anatomy in order to address any compartment dysfunction and relieve prolapse symptoms. On the one hand, when using mesh the literature tends to suggest lower prolapse recurrence rates compared to native repairs, but on the other their use has been associated with more complications such as erosion and dyspareunia. This article will focus on the classification as well as the anatomy, aetiology, presentation, investigations, and management of prolapse affecting the three different compartments. Several techniques of repair are possible in each compartment and therefore the chapter will highlight the principles of surgery, rather than be an exhaustive text of every operation available. A modification of this classification is to divide the prolapse into anatomical compartments, as defined by whether it is the anterior, apical, or posterior vaginal wall prolapse. Its simple and easy to use system has led to its common use worldwide, especially in the clinic setting. Nine measurements (in cm) are made of the position of the midline vaginal structures in relation to the hymenal ring. The advantage of this classification is Reprinted from the American Journal of Obstetrics and Gynecology, Volume 187, Issue 1, Abrams P, et al. This material is used by permission of Wiley-Liss, Inc, a subsidiary of John Wiley & Sons, Inc. Consists of four grades: grade 0-no prolapse; grade 1-halfway to hymen; grade 2-to hymen; grade 3-halfway past hymen; grade 4-maximum descent. However, its use is not yet routine as it is perceived as time-consuming, leaving its main role as a research tool when developing or comparing different surgical techniques. The most common vaginal prolapse is the anterior compartment, followed by the posterior and apical compartments.
In partial ureteric obstruction depression gifs purchase bupron sr 150mg with visa, similar but slower changes to acute obstruction are seen vital depression definition buy bupron sr with a mastercard. In neonates, this has potentially deleterious effects on tubule and glomerulus formation, compromising (though not usually causing complete loss of) renal function. In adults (dogs), Leahy showed partial obstruction for 14 days was completely reversible; 31% recovery of function was seen after 28 days of partial obstruction and only 8% function was recovered after 60 days of partial obstruction. The majority of imaging modalities rely on the anatomic finding of hydroureteronephrosis to suggest obstruction. However, dilatation of the renal pelvis may be found in the physiological conditions of high urine flow or pregnancy. Imaging options in upper urinary tract obstruction Ultrasound (kidneys, ureters, and bladder) this is a mainstay option, but is an anatomic assessment. It is noninvasive with no radiation exposure and therefore suitable in pregnancy and paediatric patients. A significant problem is that hydronephrosis is an anatomical finding and not a functional diagnosis. The finding of antenatal urinary tract dilatation should prompt a follow-up ultrasound in the first few weeks after birth to distinguish transient dilatation from more significant disease. The anteroposterior diameter of the renal pelvis is an important diagnostic tool and a diameter of greater than 50 mm is almost always associated with significant pathology. The postnatal ultrasound may give clues as to the aetiology, including whether the dilatation is unilateral or bilateral, whether the dilatation includes just the renal pelvis or the ureter and bladder, and whether there is any bladder thickening. Lower urinary tract obstruction accounts for approximately 10% of prenatally detected uropathies. Clinical presentation With the routine use of antenatal ultrasound scanning, obstructive uropathy in early life may be suggested by the finding of urinary tract dilatation. In a young child, the first presentation of obstruction may be with urinary infection or failure to thrive. Acute obstruction, such as with a renal calculus passing into the ureter, often manifests with severe colicky pain. The location of the pain can correlate with the site of urinary obstruction from proximal obstruction causing loin pain, to vesicoureteric junction obstruction causing isolated scrotal or vulval pain. Chronic progressive obstruction may be silent and found incidentally on radiological imaging or serum creatinine measurement. A patient with bilateral obstruction, or obstruction of a functionally or anatomically single kidney may describe oliguria, anuria, or uraemic symptoms. Regions of interest are drawn around each kidney and from this, a background region is subtracted to give the final renogram. The normal renogram is obtained after a bolus injection of radionuclide; however, the Rutland method is a mathematical technique which assumes a constant infusion of radionuclide from which differential uptake can be calculated. These tests involve the use of technetium (99m Tc) labelled agents to provide functional assessment of the upper urinary tract. Renal resistive indexes measured using Doppler ultrasound may help in diagnosing obstruction but suffers from an inconsistent definition of obstruction in terms of the index figure. The risk of contrast nephropathy increases with increasing serum creatinine levels and this test should not be used in patients with renal insufficiency. Retrograde pyelography this test is reserved for patients with renal insufficiency or contrast allergy risks or where the anatomy of the upper tract has not been well delineated with other imaging studies. Similarly a loopogram can be performed in people with an ileal conduit or other cutaneous urinary diversion. Antegrade pyelography this is used when all other tests have not been possible or have failed, and requires a percutaneous needle or nephrostomy and antegrade contrast injection. Whitaker test Reported in 1973,7 this test involves measurement of the renal pelvic pressure while saline or contrast is infused into the pelvicalyceal system via a percutaneous needle or nephrostomy at a steady rate of 10 mL/min. At the same time, intravesical pressure is monitored via a catheter with transducer tip. The real value is the renal pressure minus the bladder pressure: Half time of <10 minutes = normal.
However bipolar depression symptoms mania discount 150 mg bupron sr visa, excessive straining (particularly using the Valsalva manoeuvre) means pushing against a contracted pelvic floor and is counterproductive mood disorder causes order bupron sr 150 mg mastercard. The rectal contractile response to distension will then subside as the rectum relaxes and It is essential that anybody presenting with new onset of incontinence has a full history of bowel symptoms taken. The person presenting with incontinence should be able to describe when the incontinence happens, whether it is associated with the need to go to the toilet (urge incontinence), whether it is associated with walking, whether it happens at a random time (passive incontinence), and the consistency of the motions involved. Incontinence to wind is often a significant issue and may be associated with certain dietary habits. Examination should include an abdominal examination as well as a visual inspection of the perineum looking for signs of previous episiotomy or tears. Any anorectal pathology such as fistula or fourth-degree piles should be noted and the patient should be asked to strain to see how much descent of pelvic floor occurs. At the time of straining, assessment of a rectocele and cystocele can be made and this is often easier if the patient is in the lithotomy position in a gynaecological chair. Rectal examination allows the doctor to exclude faecal impaction and overflow and to assess both anal tone and squeeze pressure. It is also useful to be able to place a finger towards the vagina to see whether there is a rectocele and whether the patient has a similar sensation of pocketing as when the finger is placed within the rectocele. Measuring faecal incontinence Quantifying the degree of faecal incontinence is important to assess the outcomes of various treatment options. Faecal incontinence can be to solid, liquid, or gas and the impact on quality of life can vary greatly between patients. It is generally considered that a score of 9 or more is considered to represent significant incontinence. The Faecal Incontinence Quality of life questionnaire has 29 items and has good correlation with psychometric evaluation of symptom impact; it is more complicated and time-consuming to complete. The second study from 2010 (9) showed that lifestyle changes can improve anal incontinence in about a third of the general population. The most important things within the diet to change are those that result in loose or softer stools; these are foods that contain wheat fibre, pulses, beans, caffeine, and also lactose-containing food. There are a variety of continence aids that will help patients with faecal incontinence and the newer ones of these are anal plugs. There is, however, little in the way of evidence that these will work except in highly motivated patients. The studies that are published on plugs are relatively poor in terms of methodology. However, continence can be achieved in highly motivated patients with good compliance in up to 37% of people (10, 11). Medication One of the mainstays of treatment of faecal incontinence is the use of medication. It has an excellent safety profile and acts directly on the intestine to inhibit peristalsis increasing small intestinal and mouth-to-caecum transit time; this allows more water to be absorbed from the stool. There is some evidence that loperamide may act directly on sphincter tone and resting pressure and may increase rectal perception in healthy subjects. There was some limited evidence that antidiarrhoeal drugs may reduce faecal incontinence in patients with liquid stools. The side effects of loperamide such as constipation, abdominal pain, diarrhoea, headache, and nausea were greater than in the placebo group. A liquid form of loperamide (Imodium, paediatric) is available and is widely used by clinicians; it allows titration of symptoms with accuracy to try and reduce volume of stool and minimize side effects. Exercises and biofeedback One of the mainstays of further treatment is pelvic floor exercises, bowel training, and biofeedback. Biofeedback relies on strength training, rectal sensitivity training, and improving coordination of the rectum and anus. All four groups received patient teaching, emotional support, lifestyle modification, and a programme to explain how to manage both faecal incontinence and urge incontinence.


