Viagra
"Generic viagra 100mg with mastercard, erectile dysfunction treatment homeopathy".
By: U. Harek, M.A., M.D., Ph.D.
Assistant Professor, Northeast Ohio Medical University College of Medicine
Comparison between trained impotence testicular cancer purchase viagra overnight delivery, detrained impotence guilt purchase cheap viagra line, and untrained subjects has revealed that the training-induced decrease in -cell secretory capacity may very accurately match the accompanying increase in insulin action, because during hyperglycemic clamping glucose disposal was identical in the groups despite widely differing plasma insulin concentrations [109]. However, upon extreme athletic training oral glucose tolerance is better than in untrained subjects indicating that enhancement of insulin action is not fully compensated by reduced -cell function [109]. In athletes the sparing of insulin secretion and reduction in plasma glucose concentration are only relative to food intake; over a 24-hour period trained subjects have, compared with untrained subjects, the same overall insulin secretion and average plasma glucose concentration in the face of a higher food intake, and they also have similar blood HbA1c concentrations [109]. Accordingly, the predominant health benefit of the adaptations in pancreas and insulin-sensitive tissues resulting from intense training is that the adaptations allow the necessary increase in food intake without potentially harmful hyperglycemia and overloading of cells. To this may be added lowering of arterial insulin concentrations in consequence of the training-induced increase in hepatic insulin extraction [109]. At the other end of the activity spectrum insulin secretion and action, respectively, are also not well matched. Thus, during bedrest glucose tolerance deteriorates and glucose disposal is diminished in the face of augmented insulinemia during hyperglycemic clamping illustrating that reduction in insulin sensitivity is not fully overcome by enhancement of glucose-stimulated insulin secretion [109]. This indicates that a minimal level of physical activity is necessary for normal glucose homeostasis. In this context it should be noted that adaptations in insulin secretion and action develop rapidly upon an increase in habitual physical activity but the adaptations disappear within less than 2 weeks, if the altered lifestyle is not upheld [109,125]. The described relationships between physical activity and secretion and action of insulin also apply to the elderly [109,125,126]. Of note is the fact that the tendency for plasma insulin concentrations to increase with aging can be neutralized by a physically active lifestyle [125]. Adaptations to training in diabetics Type 1 If type 1 diabetics have a normal activity level and do not have long-term complications they also have a normal oxidative capacity of skeletal muscle and normal physical work capacity [121]. These patients generally respond to both endurance and strength training just as healthy subjects, for example by diminished heart rate and blood pressure during rest and exercise, and increased muscle force, respectively [40,121,127]. Insulin sensitivity increases and the activity of oxidative enzymes, glycogen synthase, and hexokinase increases in muscle [40,79,121,128]. Also muscle capillarization increases but the increase may be less pronounced than in healthy subjects [40,121]. However, after the honeymoon period a decrease in insulin requirements with training is not a universal finding, possibly because carbohydrate intake may increase [40,121]. Since exercise makes diabetes more difficult to control, the daily fluctuations in blood glucose may increase, and the average plasma glucose concentration, which is reflected in the HbA1c level, does not generally decline during training [40,79,121]. An improved glucoregulation is more likely to occur if patients have been poorly controlled prior to training [121], probably because training is then accompanied by more attention to disease control [79]. However, type 1 diabetic patients who participate in competitive sports may even experience deterioration of glycemic control in spite of improvements in fitness [130]. This probably reflects an irregular schedule, high exercise intensities, and measures to avoid hypoglycemia in response to exercise, that is, excessive reductions in insulin dose and excessive intake of carbohydrate. Probably reflecting the variation seen in effect of training on metabolic homeostasis some studies have found changes in plasma triglyceride and cholesterol levels upon training similar to those seen in healthy subjects, whereas other studies have not [40,121]. In agreement with this, their nonobese, nondiabetic first-degree relatives also have a low level of fitness and a high content of nonoxidative fibers in skeletal muscle [109,134]. Bedrest exacerbates the insulin resistance of obese individuals with pre-existing impaired glucose tolerance [118]. Conversely, in the postabsorptive state a single bout of prolonged submaximal dynamic [138] or resistance [139] exercise improves whole-body insulin sensitivity in type 2 diabetics. The effect of dynamic exercise has been shown to be located both in liver and peripheral tissues [138,140]. In contrast to the reaction to submaximal exercise, in response to brief intense dynamic exercise insulin sensitivity is reduced for the first 12 hours postexercise but increased after 24 hours [74]. Also in the postprandial state moderate exercise seems to increase insulin-mediated glucose disposal in the immediate postexercise period, but the effect does not persist during or after the next meal [75]. Regularly repeated exercise may increase insulin sensitivity in both elderly glucose intolerant subjects [126], women with gestational diabetes [92], and type 2 diabetic patients [136,141] and their first-degree relatives [109,134] more than can be inferred from a single bout of exercise.
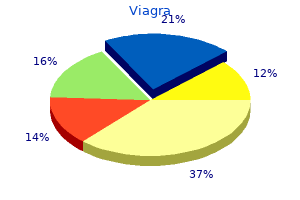
Clearly erectile dysfunction commercial bob buy generic viagra 75mg on line, future research should increasingly harness genetics as well as observational data to better determine causal risk pathways erectile dysfunction hypertension medications purchase viagra with visa. Similarly, further data are needed to better determine the extent to which insulin resistance is, or is not, linked to cardiovascular risk. However, the evidence base, as discussed in the text, is not clear as to how accurate this assumption is. Introducing insulin resistance to the clinic: the metabolic syndrome the second section of this chapter now describes how researchers and clinicians have taken commonly measured markers associated with insulin resistance and created risk algorithms which were subsequently tested for clinical utility. Different national and international organizations have produced various overlapping but different iterations of diagnostic criteria for metabolic syndrome over the last 15 years. Common to all was the requirement to fulfill three out of five criteria but not all stipulated an essential criterion. One immediate practical difficulty was the fact that fasting insulin levels were seldom measured in a routine clinical setting and that a definitive insulin resistance diagnosis was poorly defined. Importantly, the availability of various criteria for identifying metabolic syndrome and the knowledge that the relationship between risk of cardiometabolic disease and central 348 Chapter 23 Table 23. To address recognized shortcomings, a harmonized set of criteria was produced by a working group on behalf of the International Diabetes Federation Task Force on Epidemiology and Prevention, the National Heart, Lung, and Blood Institute, the American Heart Association, the World Heart Federation, the International Atherosclerosis Society, and the International Association for the Study of Obesity in 2009 [37] (see Table 23. As in previous criteria, three out of five criteria are now required to be identified as having metabolic syndrome. However, the presence of central obesity as an essential criterion was removed with the result that the presence of any three criteria now constitutes a diagnosis of metabolic syndrome. Furthermore, flexibility has been introduced into the definition of metabolic syndrome as population- and country-specific definitions for elevated waist circumference are required, reflecting the understandable lack of agreement on how best to record and define central obesity. Suggested current thresholds for elevated waist circumference, as recommended by various organizations, are provided in the document (see also Table 23. The authors propose that further research is required to properly delineate the relationship between waist circumference and cardiometabolic risk in all ethnic groups and suggest that particular health systems may even base the choice of waist circumference threshold on local considerations, including healthcare funding. Rationale for using metabolic syndrome has been summarized as: (i) facilitating research into a possible unifying pathophysiologic explanation for these strongly associated the insulin resistance syndrome 349 Table 23. Those involved in developing and promoting the concept of the metabolic syndrome have described it as a potentially valuable global public health tool with the ability to identify high-risk individuals at a young age. Undoubtedly, one positive effect of the adoption of the term has been to familiarize healthcare professionals with the potentially deleterious effects of obesity and to provide an easily understood term, or clinical label, to describe a commonly encountered type of patient. Furthermore, appreciation of those with metabolic syndrome has likely raised the profile of lifestyle advice and increased the provision of advice to those at risk of developing diabetes. Some key topics of debate have been the presence of various differing sets of criteria, now addressed by the introduction of the harmonized criteria already referred to , and the fundamental question of the role and value of metabolic syndrome in clinical practice. Some of the more humorous and incisive pieces in the medical literature in recent years have addressed this matter [4345]. In the view of many, the key question has therefore been whether identifying a patient as having metabolic syndrome yields additional predictive information on top of these risk scores. In other words, to be of clinical value, any new risk predictor must be more effective than current risk predictors to demonstrate clinical utility. It has now been well demonstrated that identification of metabolic syndrome cannot compete with the cardiovascular predictive capabilities of established cardiovascular risk scores and also that it adds minimal incremental information [5153]. To illustrate this problem with a clinical example, two theoretical but commonly encountered patients are listed in Table 23. One component, serum triglycerides, has a moderately high within-subject biologic variability of 20% with the result that classification of individuals with triglyceride levels close to 1. Other potential weaknesses include the reliance on fasting samples while there is a move towards using nonfasting sampling for both diabetes (HbA1c) and cardiovascular (lipids, HbA1c) risk estimation and diagnosis. Finally, metabolic syndrome describes relative risk of cardiometabolic disease and not absolute risk. In addition, individual components of the metabolic syndrome often outperform the overall metabolic syndrome unlike established cardiovascular risk scores [5456]. Three of the five variables in the metabolic syndrome criteria are more strongly linked to diabetes than cardiovascular disease, namely elevated triglycerides, central obesity, and dysglycemia.
Disseminated disease is usually associated with nonspecific symptoms erectile dysfunction diabetes qof viagra 100mg with visa, including fever erectile dysfunction pills for sale cheap viagra 50mg without a prescription, pallor, anorexia, and bone pain with subsequent mood changes and refusal to walk. Retro-orbital and orbital metastases are rather common, and produce a typical appearance of proptosis and periorbital ecchymoses. It is thought that an excessive inheritance of "risk" variants has been postulated that increases susceptibility to the disease. The chromosome deletions (1p, 3p, and 11q) and gains (17q) are usually associated with a poor outcome. Bone scan-Tc 99 diphosphonate scintigram is a rapid and reliable to evaluate osteolytic lesions. Histopathologically appears as "small blue round cell tumor" primitive neuroectodermal tumors which includes: 1. International Neuroblastoma pathological classification is developed by Shimada et al. Histologically, classic neuroblastomas are composed of small, primitiveappearing cells with dark nuclei, scant cytoplasm, and poorly defined cell borders growing in solid sheets Mitotic activity, nuclear breakdown ("karyorrhexis"), and pleomorphism may be prominent. The background often demonstrates a faintly eosinophilic fibrillary material (neuropil) that corresponds to neuritic processes of the primitive neuroblasts, demonstration of small, membranebound, cytoplasmic catecholamine-containing secretory granules. Typically, rosettes (Homer-Wright pseudo-rosettes) can be found in which the tumor cells are concentrically arranged about a central space filled with neuropil. Other helpful features include immunochemical detection of neuronspecific enolase, neurofilament protein, S100. Neuroblastoma Staging System International neuroblastoma staging system are depicted in Table 16. Low-risk Neuroblastoma Survival rates for patients who have stage 1 disease, regardless of biologic factors, are excellent with surgery alone. Chemotherapy, when necessary, has been an effective salvage therapy for patients who have stage 1 disease and relapse after surgery only. Chemotherapy or low-dose radiotherapy is reserved for patients who have large tumors or massive hepatomegaly causing mechanical obstruction, respiratory insufficiency or liver dysfunction. Intermediate-risk Neuroblastoma the intermediate-risk classification group encompasses a wide spectrum of disease. Standard therapy for patients who have high-risk neuroblastoma involves at least four components: Induction, local control, consolidation, and treatment of minimal disease with biologic agents. An alternative induction strategy is to add noncross-resistant cytotoxic agents into this multiagent chemotherapy backbone. The topoisomerase I inhibitor class of agents, including topotecan, has activity in recurrent neuroblastoma and can be safely combined with multiagent induction chemotherapy. Local Control Optimal local control is achieved with a combination of aggressive surgical resection and administration of external-beam radiotherapy to the primary tumor site regardless of response to induction chemotherapy. Resection of the primary tumor and bulky metastatic disease is usually necessary to achieve a chance of cure. Delayed surgical resection after initial induction chemotherapy improves resection of the primary tumor, may improve overall survival, and may minimize acute complications of surgical resection. The presence of residual tumor at the time of radiation therapy affects risk for recurrence. Myeloablative Consolidation Therapy the studies have demonstrated that myeloablative therapy with purged bone marrow transplant improved outcome for patients who had high-risk neuroblastoma. Epidemiology the approximate incidence is 35 cases per million in children under 15 years of age. The etiology is unknown but there is some predilection in the following conditions: 1. General Signs and Symptoms of Intracranial Tumors the common signs and symptoms are grouped in Table 17. The signs and symptoms depend upon the size, location and growth rate of the tumor. Slow growing tumors are usually large at presentation and on the other hand rapidly growing tumors present early when they are small. Diplopia (6th nerve palsy): In young children diplopia may present as frequent blinking or intermittent strabismus. Parinaud syndrome (failure of upward gaze and setting-sun sign, large pupils and decreased constriction to light). Mental disturbances: Somnolence, irritability, personality or behavioral change, or change in school performance.
The relative prevalence varies erectile dysfunction quick natural remedies buy viagra on line amex, by country erectile dysfunction medication shots purchase discount viagra on line, according to how patients are identified. Over 200 different heterozygous loss-of-function mutations have now been described, all causing a similar clinical picture. Homozygous loss-of-function glucokinase mutations are a rare cause of insulin-requiring diabetes presenting in the neonatal period [11]. There is maintained glucose homeostasis as shown by the small increment in plasma glucose at two hours during an oral glucose tolerance test, albeit at a higher set point than in normal subjects [15]. The incidence of macrovascular complications appears similar to the background population. A correct diagnosis is important in young people who might otherwise be thought to have type 1 diabetes. The aim of treatment of diabetes in pregnancy is to minimize the risk of fetal and maternal complications. In this latter setting, aggressively lowering maternal glycemia may adversely affect fetal growth [19]. As it is not usually possible to determine the fetal genotype, the decision on whether to treat the mother should be based on fetal growth. Transcription factors have an important role in regulating the expression of genes. They have a critical role in the variations in gene expression in the different stages of embryological development, and in different tissues. Transcription factors can also regulate expression of other transcription factors, thus establishing a complex regulatory network controlling gene expression. It has been hypothesized that this feedback loop acts as a bistable switch that is only stable fully on or fully off. Mouse studies [31,35] suggest that the deterioration is due to a decrease in -cell mass with time. Nearly 200 mutations have been found scattered throughout the gene and consist of frameshift, missense, nonsense, and splice site mutations. Transcription factor mutations alter insulin secretion in the mature cell as well as altering -cell development, proliferation, and cell death. Over 40 mutations have been described with the majority in the first four exons of the gene [23]. Hence glycosuria can occur at relatively mild levels of blood glucose (<8 mmol L-1). Renal glycosuria has been shown to precede the development of diabetes and makes the screening of at-risk children by urinary screening for glycosuria an appropriate and sensitive screening test. Frequency of microvascular complications is similar to that seen in type 1 and type 2 diabetes and relates to degree of glycemic control [38]. There is on average an 800 g increase in birth weight compared with nonmutation-carrying siblings [39]. These features appear to relate to increased insulin secretion in utero and in early infancy which evolves into reduced insulin secretion and diabetes in later life [39]. In those without diabetes, it is usually sufficient to screen for diabetes using fasting plasma glucose. When commencing oral agents the sensitivity to sulfonylureas means that these are the treatment of choice [43]. The starting dose should therefore be low-we use a starting dose of 40 mg gliclazide daily in adults. If there is hypoglycemia with low doses of sulfonylurea a short-acting agent such as nateglinide may be appropriate [44]. In those patients on treatment for a pre-existing diagnosis of type 1 or type 2 diabetes, the aim should be to switch to treatment with a sulfonylurea (if this is not already the case). As with all pregestational diabetes prenatal counseling is sensible to discuss and optimize treatment. Given the greater clinical experience and pregnancy safety data with glibenclamide (glyburide) we recommend that women switch to this sulfonylurea prior to conception. Given this, pregnancies need close monitoring with: very tight glucose control in mothers with diabetes; frequent fetal ultrasounds to monitor growth; early (even preterm) planned delivery if evidence of macrosomia; and monitoring of the newborn for hypoglycemia with consideration of diazoxide treatment, if hypoglycemia persists, according to published guidelines [47]. Clinical features Patients may be detected when glucose is tested in the first few days of life in low-birth weight babies or may present later when the patient is severely unwell with ketoacidosis.
Consequently erectile dysfunction and diabetes pdf cheap 25mg viagra free shipping, the -cell dose-response relating insulin secretion to glucose concentration is shifted upwards (c) erectile dysfunction doctors raleigh nc purchase viagra cheap. Normal -cell function 113 Insulin secretion that is, the increase in insulin secretion is higher when glucose concentration is higher, whereas at low glucose the amplification is marginal. The relationship between the levels of incretin hormones and the incretin effect are in fact generally weak [38,47,48]; whether this is due to limited assay precision or factors other than the hormone levels remains to be clarified. Therefore, based on this analysis the contribution of early secretion phenomena is quantitatively limited during an oral glucose load as well. The response to oral glucose is also characterized by phenomena that enhance -cell glucose sensitivity during the test, referred to as "potentiation. The -cell dose-response explains most of the insulin secretion excursions (bottom, gray line). However, in the initial period insulin secretion is relatively higher (bottom, horizontally banded area); this anticipative response accounts for 1015% of the total suprabasal secretion. However, some studies have reported that the -cell dose-response does not remain the same during the 24 hours. In particular, in relation to the glucose levels insulin secretion is relatively potentiated during the morning meal and attenuated during the following meals and the night, to a significant extent [20,50]. After the ingestion of a small amount of proteins (3050 g) [51,55] or a larger amount of proteins (2 g kg-1) [56], plasma insulin was raised two- to threefold over baseline and remained persistently elevated for 90 or 240 minutes, respectively. In support of this hypothesis, it has been shown that insulin response to different protein solutions was closely related to the increase of plasma amino acids [5759] with large differences among the individual amino acids unexplained by the functional group [60]: phenylalanine and glycine shown to be the most potent (+30 pmol L-1), histidine, tyrosine, and, surprisingly, arginine as neutral, and the others as intermediate (+10. In vitro studies [61] have reported that the insulinotropic effect of amino acids is mostly dependent on the amino acid type, duration of exposure and concentration; furthermore only combination of amino acids stimulates insulin secretion when added at physiologic concentrations, whereas higher concentrations of individual amino acids are required to activate insulin secretion [61]. Accordingly, the intravenous administration of a relatively small number of amino acids individually promotes insulin release while the maximum stimulus is elicited by mixed amino acids [62]. In contrast to other amino acids, homocysteine in vitro showed a dose-dependent negative effect on insulin secretion in pancreatic cells [63]. When either amino acids or proteins were ingested with glucose, plasma insulin levels were not significant or only slightly different from those after oral glucose alone but at lower glucose concentration [5255,59,60,64,65] suggesting a direct effect on -cell glucose sensitivity. A 2448-h lipid infusion has been reported to reduce [78], increase [79] or not significantly change [80] glucose-induced insulin secretion. Slow -cell response modes and adaptation mechanisms the secretion mechanisms discussed above are relatively rapid and typically suited to coping with the insulin needs of a meal. The healthy cell can also respond with slower modes, adapting to insulin demand if required by the metabolic conditions. Glucose-induced potentiation of insulin secretion Slow response modes are unveiled by prolonged exposure to hyperglycemia or repeated glycemic stimuli. During a hyperglycemic clamp, particularly at high glucose levels (>10 mmol L-1), the second-phase response exhibits a slow progressive rise over time [23]. When two consecutive hyperglycemic episodes are brought about, the insulin response after the second one is higher compared to the first [11]. With a prolonged (three day) infusion of glucose at a low constant rate, the insulin response assessed with a hyperglycemic clamp before and after the infusion is increased more than twofold [93]. Similarly, a prolonged glucose infusion makes the -cell dose-response, assessed with the graded glucose infusion test, steeper [22]. When glucose is infused intravenously to mimic the response to an oral glucose test, increasing glucose doses and concentrations produces an upward shift of the -cell dose-response, that is, insulin secretion becomes greater for the same glucose level [38]. The common denominator of these phenomena is that sustained hyperglycemia potentiates insulin secretion; this mechanism provides an additional resource to control glucose levels. Normal -cell function 115 Another classical experiment showing the potentiating effect of exposure to hyperglycemia involves the use of arginine as a secretagogue. When the arginine bolus is administered in a hyperglycemic state created by a hyperglycemic clamp, the insulin secretion response is potentiated compared to the basal state [94]. In normal subjects, the magnitude of this potentiation increases almost in proportion to the glucose levels until it reaches a plateau above 30 mmol L-1 glucose, where the response to arginine is more than fivefold the response at basal glucose. The initial slope of this curve, denoted as the glucose potentiation slope, is an index of the ability of glucose to potentiate insulin secretion [94]. Adaptation to insulin sensitivity A widely studied adaptive mechanism of the cell is the modulation of its response by prevalent insulin sensitivity.