Olanzapine
"Cheap 2.5mg olanzapine otc, treatment ear infection".
By: E. Joey, M.A., M.D.
Program Director, Georgetown University School of Medicine
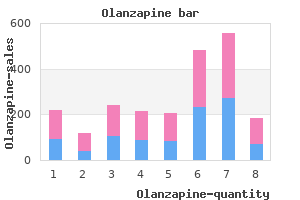
Similarly medicine xalatan buy 7.5mg olanzapine with amex, hepatic destruction from sickle cell disease symptoms sinus infection order on line olanzapine, tumor necrosis (either spontaneous or following iatrogenic embolization), or cirrhosis can predispose to abscess formation. Host factors that predispose to abscess formation from "routine" hepatic bacterial insults may be present in many cryptogenic abscesses. Systemic illness such as diabetes mellitus, cardiopulmonary disease, malignancy, and cirrhosis are common in patients with liver abscesses and may be predisposing factors. Diabetes was shown in one retrospective study to impart a greater than threefold risk of development of pyogenic liver abscess. For example, one-third of patients with chronic granulomatous disease followed at the National Institutes of Health Clinical Center over four decades developed pyogenic liver abscesses; 47% had recurrent abscesses. Most individuals experience asymptomatic infection, but approximately 10% develop symptomatic colitis when invasion of the colonic mucosa occurs. Pyogenic liver abscesses are usually classified by presumed route of hepatic invasion: (1) biliary tree, (2) portal vein, (3) hepatic artery, (4) direct extension from contiguous focus of infection, and (5) penetrating trauma. Ideally, this approach defines the microbiology of the abscess and therefore guides empirical antibiotic choice, but it is limited by the high frequency of cryptogenic abscesses. The frequencies of the presumed routes of hepatic invasion are presented in Table 75. In all cases, the liver and intestinal amebae had discordant genotypes, suggesting either that amebae undergo genetic reorganization during invasion or that only a subset of strains is capable of metastasizing to the liver. Microbiology Amebic Liver Abscess Pyogenic Liver Abscess In light of the diverse pathologic processes that have been discussed, it is understandable that sweeping generalizations about the microbiology of pyogenic liver abscess are difficult. The picture is further complicated because abscess material is rarely obtained before the administration of antibiotics. Even in the preantibiotic era, a high rate of sterile cultures was seen, probably reflecting inadequate culture techniques. There has also been an increased appreciation that many liver abscesses are polymicrobial, with estimates ranging from 20% to 50%, depending on the case series. If the source of the abscess is considered, abscesses with a biliary source are most likely to be polymicrobial, and cryptogenic abscesses are most frequently monomicrobial. In the first, a synergistic combination of organisms converges by chance to form a single abscess, and in the second, a highly pathogenic organism forms abscesses wherever it was seeded. The latter has been increasingly recognized as a cause of community-acquired monomicrobial liver abscesses (discussed later). Enterococci and viridans-group streptococci are also common, primarily in polymicrobial abscesses. Staphylococcus aureus, by contrast, is more commonly associated with monomicrobial abscesses. Although pyogenic liver abscesses due to fungi, particularly Candida species, have been reported, they are comparatively rare and are excluded from most case series. Cough Jaundice Right upper quadrant tenderness Laboratory Tests (Approximate % of Cases) Leukocytosis Elevated alkaline phosphatase Solitary lesion 80 80 70 75 65 70 infections such as meningitis and endophthalmitis occur in 10% to 16% of all cases. Mutagenesis of one cps gene, magA (for mucoviscosity-associated gene A), abolishes hypermucoviscosity, increases sensitivity to phagocytosis and serum-mediated lysis, and reduces virulence in mice. Only 15% to 35% of patients present with concurrent gastrointestinal symptoms, including nausea, vomiting, abdominal cramping, and diarrhea (Table 75. Corticosteroid use and male sex are well-established risk factors for invasive amebic disease. Only 1 patient in 10 presents with the classic triad of fever, jaundice, and right upper quadrant tenderness. Fever is common, often without localizing signs but only with a general failure to thrive, including malaise, 1040 fatigue, anorexia, or weight loss (see Table 75. When present, localizing symptoms such as vomiting or abdominal pain are not specific. The duration of symptoms before presentation varied widely in most case series, and there was seldom agreement on an average duration.
Other infectious causes of eosinophilic meningitis include Gnathostoma species medicine x xtreme pastillas purchase discount olanzapine on line, Baylisascaris procyonis treatment wasp stings discount olanzapine express, Toxocara species, and Taenia solium. After viremia, viral particles are normally cleared by the reticuloendothelial system, with the speed of removal directly related to virus size. Some viruses directly infect cerebral microvascular endothelial cells before infection of adjacent glia and neurons,182,183 whereas others initially infect glia without evidence of endothelial cell infection. Studies of mumps virus in hamsters have shown a sequence of infection from the choroid plexus to the ependyma to parenchymal cells; viral nucleocapsids have been found in the choroid plexus and ependymal cells of humans with mumps meningitis. Viremia and Central Nervous System Invasion Chapter 87 Acute Meningitis After the colonization of selected mucosal surfaces in the body by various viruses, the host possesses numerous barriers to prevent viral entry. Gastric acidity inactivates most swallowed viruses, and gastrointestinal enzymes and bile also disrupt viral envelopes, capsid proteins, and lipoprotein membranes; however, some nonenveloped, acid-resistant viruses. When the host has had previous contact with the viral agent, the mucosa of the gastrointestinal and respiratory tracts may be coated with secretory immunoglobulin A (IgA), which neutralizes the virus and prevents attachment and subsequent cell penetration. Experimental evidence supports each mode of transit, and all may be involved to various degrees in different viral infections. Sensitized lymphocytes probably respond to a virus-specific protein that diffuses or is transported to the luminal surface of the endothelium, with subsequent passage through endothelial cells and release of inflammatory cytokines. Failure of an immune response to develop may be a result of immunologic tolerance, host immune defects, or the ability of the virus to escape immune surveillance. The initiation of infection with meningeal pathogens usually begins with host acquisition of a new organism by nasopharyngeal colonization. Studies have provided more information on the pathogenesis of meningococcal invasion. This observation suggests that although fimbriae play an initial role in adherence of H. In an experimental infant rat model, it was demonstrated that although all encapsulated strains of H. Indeed, antibodies to type b capsule, which are almost uniformly detected in humans by the age of 4 years even in the absence of known exposure to H. Polysaccharide capsule may also be an important virulence factor for the development of invasive disease by S. In addition, in vivo capsular transformation events may equip pneumococcal strains with highly virulent bloodinvasive phenotypes, thereby increasing the seriousness of pneumococcal infection, especially that caused by multidrug-resistant strains. However, it appears that the presence of high concentrations of circulating IgA antibodies to N. However, the exact role of IgA protease production in this pathogenic sequence remains unclear. The presence of anticapsular polysaccharide antibodies may also be effective in decreasing nasopharyngeal carriage of meningeal pathogens. In an intralitter transmission model in which infant rats were intranasally inoculated with S. Once bacteria cross the mucosal barrier and gain access to the bloodstream, they must overcome additional host defense mechanisms to survive. The presence of bacterial capsule, by effectively inhibiting neutrophil phagocytosis and resisting classical complement-mediated bactericidal activity, may enhance bloodstream survival of the organism, thereby facilitating intravascular replication. In addition, certain capsular types are disproportionately associated with the development of meningitis. Presence of the K1 capsule and a high degree of bacteremia are key determinants in the development of E. The host possesses several defense mechanisms to counteract the antiphagocytic effects of the bacterial capsule. Experimental studies in a rat model have shown that after intravenous or intraperitoneal challenge with H. Although the incidence of bacteremia caused by type b organisms increased from 63% to 95% in complement-depleted rats, the incidence and severity of meningitis were unaffected by complement depletion. In an experimental study of pneumococcal meningitis in mice and rats, complement inhibition by C1 inhibitor was associated with reduced clinical illness, a less-pronounced inflammatory infiltrate around the meninges, and lower brain concentrations of proinflammatory cytokines and chemokines. Patients with deficiencies in the membrane attack complex are particularly prone to neisserial infections, although usually with a more favorable outcome when appropriate therapy is instituted.
Efficacy and safety of cefotaxime in combination with metronidazole for empirical treatment of brain abscess in clinical practice: a retrospective study of 66 consecutive cases medications via endotracheal tube order genuine olanzapine on line. May short-course intravenous antimicrobial administration be as a standard therapy for bacterial brain abscess treated surgically Successful treatment of brain abscess caused by Nocardia in an immunocompromised patient after failure of co-trimoxazole medicine grace potter order olanzapine 2.5mg with mastercard. Successful treatment of disseminated nocardiosis complicated by cerebral abscess with ceftriaxone and amikacin: case report. Intracerebral Nocardia asteroides abscess treated by neurosurgical aspiration and combined therapy with sulfadiazine and cefotaxime. Nocardia asteroides cerebral abscess in immunocompetent hosts: report of three cases and review of surgical recommendations. Successful long-term treatment of cerebral nocardiosis with unexpectedly low doses of linezolid in an immunocompromised patient receiving complex polytherapy. Myelosuppressionsparing treatment of central nervous system nocardiosis in a multiple myeloma patient utilizing a tedizolid-based regimen: a case report. Primary Nocardia farcinica brain abscess with secondary meningitis and ventriculitis in an immunocompetent patient, successfully treated with moxifloxacin. A review of brain abscess surgical treatment-78 years: aspiration versus excision. Surgical outcome of encapsulated brain abscess in superficial non-eloquent area: a systematic review. Nocardial cerebral abscess: report of three cases and review of the current neurosurgical management. Candida albicans brain abscesses in a premature infant treated with amphotericin B, flucytosine and fluconazole. Failure of caspofungin to treat brain abscesses secondary to Candida albicans prosthetic valve endocarditis. Antifungal and surgical treatment of invasive aspergillosis: review of 2,121 published cases. Disseminated invasive aspergillosis with cerebral involvement treated with caspofungin and voriconazole. Cerebral aspergillosis in the critically ill: two cases of successful medical treatment. Rapid improvement of disseminated aspergillosis with caspofungin/voriconazole combination in an adult leukemic patient. Use of posaconazole delayed-release tablets for treatment of invasive aspergillosis. Rhinocerebral mucormycosis: results of aggressive surgical debridement and amphotericin B. Posaconazole is effective as salvage therapy in zygomycosis: a retrospective summary of 91 cases. Rhinocerebral mucormycosis with cerebral extension successfully treated with adjunctive hyperbaric oxygen therapy. Cerebral Rhizomucor infection treated by posaconazole delayed-release tablets in an allogeneic stem cell transplant recipient. Treatment of scedosporiosis with voriconazole: clinical experience with Chapter 90 Brain Abscess 1261. Scedosporium prolificans brain abscess in a patient with chronic granulomatous disease: successful combination therapy with voriconazole and terbinafine. Combination of amphotericin B and flucytosine against neurotropic species of melanized fungi causing primary cerebral phaeohyphomycosis.
The mechanism of macrolideassociated improvement in lung disease is still uncertain medicine 1975 lyrics purchase olanzapine 5 mg online, but azithromycin is thought to modulate inflammation and may in fact have some direct antimicrobial impact medications errors order 2.5mg olanzapine free shipping. Despite an increase in drug resistance, there was no significant impact of emergent drug resistance on lung function. A number of other inhaled antibiotics are in various phases of active clinical trials, including inhaled levofloxacin and vancomycin. Prolonged or continuous infusion of -lactam antibiotics has been utilized with more frequency. Though the study did not achieve it primary outcome, this was likely due to lack of reliable outcome measures in this age group. Given susceptibility data in particular patients, how should providers go about selecting antibiotics and what is the optimal length of therapy The multicentered study revealed substantial variation in treatment duration and regimen. In addition, patients with acute pulmonary infections should be tested for respiratory viruses, especially during influenza season. While there is still hope for traditional gene therapy, recent advances in gene editing have demonstrated real promise. High-throughput screening of small molecules helped launch a new treatment paradigm. Once-daily tezacaftor, in combination with twice-daily ivacaftor, was introduced as an alternative to lumacaftor and led to a similar but slightly greater improvement in lung function. Next-generation correctors to complement tezacaftor-ivacaftor have demonstrated significantly superior outcomes in comparison to tezacaftor-ivacaftor alone. These effective therapies provide an opportunity to study the change in microenvironment and airway surface liquid of the lung and its impact on bacteria infecting the airways. Sustained Benefit from ivacaftor demonstrated by combining clinical trial and cystic fibrosis patient registry data. Pseudomonas aeruginosa (Pa) positivity among those with a recorded respiratory culture in 6-month intervals. Clinical mechanism of the cystic fibrosis transmembrane conductance regulator potentiator ivacaftor in G551D-mediated cystic fibrosis. Though some nonsense mutations may respond to small-molecule modulators, the great majority will require a different treatment paradigm that may also apply to other genetically inherited orphan diseases. As with all patients, health care providers should perform hand hygiene with an alcohol-based hand rub, or with antimicrobial soap and water, when hands might be contaminated with pathogens. Most early infections in lung transplant recipients are surgical site infections associated with the pleural space, fractured ribs, or soft tissue and, more rarely, anastomotic site infections. As part of the pretransplantation evaluation, all recent respiratory tract bacterial isolates are taken into consideration in preparing a tailored perioperative antimicrobial regimen. This antibacterial regimen is continued for 2 weeks postoperatively and is adjusted by dayof-transplant bronchial cultures obtained from the recipient and donor. All patients receive inhaled colistin or tobramycin during their initial hospitalization to minimize the risk of anastomotic site infection. A majority of lung transplantation centers adopted "universal" prolonged voriconazole prophylaxis when this antifungal was approved in 2002. Although this has probably led to lower incidence of fungal 961 disease, most chronic toxicities of voriconazole use have been described in this population, especially phototoxicity, and periostitis probably from voriconazole-associated fluorosis. Analysis of fungal disease epidemiology in lung transplantation patients at our center pointed to the fact that most fungal disease was related to perioperative contamination with Candida and Aspergillus, and was not a result of increased immunosuppression. Given these data, we implemented a "targeted" strategy in which all patients receive micafungin as part of their perioperative antimicrobial regimen, beginning with induction of anesthesia and continued for 7 to 10 days. Patients also received inhaled amphotericin twice daily during their initial hospitalization or if they receive treatment for acute rejection. Once the explant pathology and day-of-transplant cultures are available, patients who had positive cultures for yeast or molds are treated with fluconazole or voriconazole, depending on fungal species isolated and susceptibilities, and are continued on this regimen for 3 to 6 months. With this strategy, around 10% of transplanted patients go home on voriconazole, and the incidence of fungal disease is comparable to centers that use "universal" strategies. This requires judicious interpretation of cultures obtained during surveillance bronchoscopies, since cultures may represent oral or sinus contamination at the time of the procedures.
The most important infecting microorganism in septic cavernous sinus thrombosis is S treatment 4 high blood pressure purchase olanzapine pills in toronto. Lateral sinus thrombosis complicating mastoiditis continues to be a problem in the postantibiotic era symptoms ruptured spleen buy olanzapine 7.5 mg free shipping. The clinical manifestations may relate to damage to the nerves that traverse the cavernous sinuses. The most common symptoms in patients with septic cavernous sinus thrombosis are headache, fever, and diplopia110,122; headache is more common if the antecedent condition is sinusitis rather than a facial infection. Papilledema or venous engorgement is observed in 65% of patients, and a change in mental status in 55%. Meningismus is present in up to 40% of patients, usually secondary to retrograde spread of the thrombophlebitis. Less than 50% of patients have dilated or sluggishly reactive pupils, decreased visual acuity (which may progress to blindness), and dysfunction of cranial nerve V. As infection spreads to the opposite cavernous sinus through the intercavernous sinuses, findings are duplicated in the opposite eye, usually within 24 to 48 hours after the initial unilateral periorbital edema. Carotid artery inflammation and cortical vein thrombophlebitis are particularly serious complications of septic cavernous sinus thrombosis because they carry the risk of cerebral hemorrhagic infarction. In contrast, in the more indolent form of cavernous sinus thrombosis, which usually occurs secondary to dental infection, otitis media, or paranasal sinusitis, the orbital manifestations are often unimpressive and involvement of the contralateral eye is a late and inconsistent finding. The presentation in patients with septic lateral sinus thrombosis is typically more gradual, and patients complain predominantly of headache (>80% of cases); photophobia, earache, vomiting, and vertigo may also occur because otitis media is a common predisposing condition. Posterior auricular swelling and pain (Griesinger sign) are present in almost 50% of cases; a common complication is otitic hydrocephalus. In one study of 13 patients, the majority exhibited cranial neuropathies and raised intracranial pressure. Thrombosis of the superior sagittal sinus produces an abnormal mental status, motor deficits, nuchal rigidity, and papilledema. The majority of cases occur in the setting of bacterial meningitis, in which the onset may be fulminant. Patients with sinusitis as a predisposing condition tend to have a subacute onset of symptoms. Laboratory studies are usually nonspecific in suppurative intracranial thrombophlebitis. Blood cultures may be positive, especially in patients with a rapidly progressive course. Chest radiographs may reveal evidence of septic pulmonary emboli after propagation of the thrombus into the inferior petrosal sinus and jugular vein. Magnetic resonance venography is extremely useful in showing detailed venous anatomy and demonstrating an area of decreased or absent signal in the area of the thrombus. Selection of appropriate antimicrobial therapy for suppurative intracranial thrombophlebitis depends on the antecedent clinical condition; the likely microorganisms are similar to those observed in cranial subdural empyema and cranial epidural abscess (see earlier discussions). If the antecedent clinical condition is paranasal sinusitis, empirical antimicrobial therapy should be directed toward staphylococci, streptococci, aerobic gram-negative bacilli, and anaerobes. In septic cavernous sinus thrombosis, an antistaphylococcal agent should always be included because of the high likelihood of isolation of S. Vancomycin is recommended empirically, pending results of in vitro susceptibility testing. An appropriate empirical regimen is vancomycin, metronidazole, and a third- or fourth-generation cephalosporin, pending culture results and in vitro susceptibility testing. Intravenous antimicrobial therapy is usually continued for at least 3 to 4 weeks, but the duration needs to be individualized depending on the clinical response. The role of corticosteroids is not well established in the management of septic cerebral venous thrombosis; although they may help in decreasing inflammation and swelling, this use is not well supported by evidence. In fact, some authors have recommended operative intervention for all patients who develop cavernous sinus thrombosis as a complication of sinusitis. Arrow points to contrast-enhanced cavernous sinus with a dark circle of a flowing carotid artery (flow void signal).

