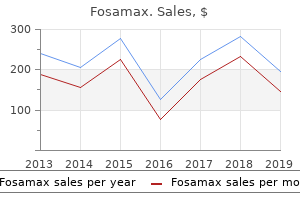
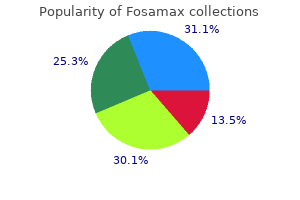
Fosamax
"Buy fosamax 35 mg cheap, womens health institute taos nm".
By: K. Pedar, M.A.S., M.D.
Co-Director, Albert Einstein College of Medicine
Full range of the cervical spine may then be tested: flexion menstruation or period generic fosamax 35 mg online, extension menopause japan purchase fosamax australia, rotation, and lateral bending. During rotation and lateral bending, ipsilateral discomfort elicited in the direction of movement is suggestive of bony pain. Pain and/or tightness produced on the contralateral side usually implicate a muscular disorder. Finally, palpable tenderness of the spinous processes may indicate bony pathology, whereas local tenderness of paraspinous muscles usually indicates myofascial pain. Passive range of motion (and provocative tests) should not be performed if instability or fracture of the cervical spine is suspected. What is the value of provocative tests for diagnosing cervical radiculopathy due to nerve root compression within the foramina of the cervical vertebrae Provocative maneuvers vary in their sensitivity and specificity for diagnosing cervical radiculopathy. The sensitivity for each of the tests is approximately 30% lower for chronic cervical radiculopathy. The immediate development of pain and/or paresthesias with radiation to the upper limb (see below) is indicative of cervical radiculopathy; sensitivity 45% to 55% and specificity 85% to 93%. The test is considered positive if this position relieves the radicular pain; sensitivity 45% to 55% and specificity 85%. Reproduction of symptoms is positive; sensitivity 60% to 80% and specificity 20% to 40%. Test considered positive if radicular pain is improved; sensitivity 44% and specificity 95%. Reproduction of radicular symptoms is a positive test; sensitivity 22% and specificity 94%. What physical findings enable you to identify the approximate level of common, cervical nerve root lesions Nerve C5 (5%) C6 (35%) C7 (35%) C8 (25%) T1 (rare) aAttributing bRadial Sensory Loss Lateral upper arm Lateral forearm, thumb, index finger Middle finger Medial forearm, ring finger, little finger, Medial arm at elbow Motor Weaknessa Deltoid, biceps Wrist extensors, biceps Wrist flexors, finger extensors, triceps Finger flexors, thumb extensor, hand intrinsics Finger abductors Reflex Biceps Radialb, biceps Triceps None None weakness of upper extremity muscles to a specific cervical level is often difficult since innervations usually occur by two or more nerve roots. List the important questions that should be asked when obtaining a history from a patient with low back pain. One can use the helpful mnemonic P-Q-R-S-T (the components of an electrocardiogram tracing) when approaching any patient with pain: P-Provocative and palliative factors: sitting (worse with discogenic), walking (worse with spinal stenosis-relieved with forward flexion), supine (pain unrelieved if cancer or infection), Valsalva maneuver (worse with intrathecal or radicular process), lumbar extension (worse with spinal stenosis and facet arthritis) versus flexion (worse with lumbar strain or fibromyalgia). What is the position of maximal comfort, and does this reduce or eliminate pain or radicular symptoms R-Radiation of pain: into leg (radicular), saddle area with bowel/bladder dysfunction (cauda equina syndrome), bilateral buttock or thigh (spinal stenosis, ankylosing spondylitis, or referred from intraabdominal pathology) S-Severity of pain and systemic symptoms: pain scale 1 to 10; fever, weight loss, change in bowel habits, etc. There are sensory nerve fibers in the discs, vertebral end plates, facet joints, ligaments, fascia, blood vessels, spinal nerve roots, and muscles surrounding the lumbar spinal column. Therefore, nonspecific mechanical low back pain could originate from any one or combinations of these sites. Most low back pain is mechanical in nature and should slowly improve over 2 to 6 weeks. As such, the presence of red flags may not be associated with worrisome pathology in a patient with acute onset back pain, especially if it is improving. Potential exceptions include older age, history of steroid use, trauma, and/or presence of a contusion overlying the site of back pain. In patients presenting with chronic low back pain (3 months), however, the presence of red flags may be more concerning for underlying pathology. Obtaining imaging studies and additional work-up on every patient with a red flag sign or symptom is controversial and may lead to costly evaluations for a common condition. The simplest definition of sciatica is back pain that radiates down one leg below the knee. Occasionally, dermatome numbness and paresthesias of the lower limb are also reported. Valsalva maneuvers or flexion and extension of the lumbosacral spine may exacerbate these symptoms.
This maltracking leads to increased pressure on the lateral facet of the patella and pain breast cancer zazzle purchase cheapest fosamax and fosamax. It is common in young adults and responds to directed rehabilitation of the quadriceps and stretching of the hamstrings women's health issues in louisiana order discount fosamax online. Other common conditions that affect the patella and give rise to anterior knee pain are true patellar malalignment, limb malrotation, and tendinitis. One should always evaluate the patient for pes planus with foot pronation to see if this is contributing to patellar maltracking. This may be due to multiple factors including anatomy, hormones, and neuromuscular imbalance. It is performed by applying a valgus and internal rotation force on the tibia with the knee in full extension and hip abducted 10 to 20 degrees. A clunk of tibial rotation is appreciated as the knee passes 20 to 40 degrees of flexion. The appreciable clunk occurs when the tibia, which is abnormally subluxated (anterior and internally rotated), is pulled back into its normal position by the secondary restraints. The meniscus functions as a cushion between the femur and tibia on the medial and lateral sides of the knee. It is well suited to compression but tears when subjected to shear stress with a turning or twisting motion. The nutrition of the inner two-thirds of the meniscus is limited and predisposes the torn tissue to not heal once torn, a factor reflected by the typical chronic recurring history of symptoms. The torn tissue may create a mechanical block to the free motion of the knee, which will symptomatically manifest as clicking, popping, and locking, and is associated with pain and swelling at the joint line. Joint line tenderness is one of the best clinical signs of a meniscal tear, but all of these tests should be combined with the history as the presentation of a meniscal tear can be confused with patellofemoral pathology, particularly in the absence of a single precipitating event. Chronic degenerative meniscal tears can oftentimes be treated with physical therapy alone. This combination is almost always a result of sporting activities, particularly a valgus impact to the knee with the foot firmly planted. The knee in these injuries exhibits a markedly positive anterior drawer test, a positive Lachman test and pivot shift test, and marked valgus angulation with applied stress in full extension. The knee will be stable to varus stress testing because the lateral collateral ligament and posterior cruciate ligament remain intact. Effusion from hemarthrosis may be mild secondary to medial capsular tearing, which allows the traumatic bleeding to exit the knee joint. Suspicion of an injury of this magnitude should lead to the prompt referral to an orthopedic surgeon. The lateral ligaments (anterior talofibular and calcaneofibular) are the most commonly involved. An injury to the anterior tibiofibular syndesmosis is referred to as a "high ankle sprain" and is more severe requiring more time for recovery. Eversion injuries are less common but involve injury to the medial deltoid ligament. Name two lower extremity tendons susceptible to overuse injuries occurring in runners. Acute Achilles tendon rupture usually results from a forced contraction of the gastrocnemius muscle against resistance, which occurs either during sports participation or from a fall. The patient usually has symptoms of pain, most notable in walking, and weakness in the push-off phase of gait. A positive Thompson test is common oftentimes with a palpable defect in the tendon. Options include closed treatment with placement in a long or short leg cast with the foot in equinus (plantar-flexed by gravity). A percutaneous suture repair has been reported with good results but may risk some injury to the sural nerve. The most recent literature reports that the closed technique is equivalent to surgical intervention with the advent of early functional rehab and modern reports of re-rupture rates are similar between the two groups. Some studies do show earlier and better restoration of calf strength with surgical intervention. Therefore, selection of the best treatment option is individualized, with age, activity level, patient and surgeon interests, and experience as guiding parameters.
Chronic infections by mycobacteria and fungi often cause radiographically detectable abnormalities women's health center tampa general hospital buy 70mg fosamax mastercard. Osteoarthritis breast cancer kd shoes fosamax 70 mg with visa, avascular necrosis of bone, and other causes of noninflammatory chronic arthritis also have characteristic radiographic appearances. A bloody synovial effusion points to pigmented villonodular synovitis, synovial chondromatosis, synovial sarcoma, or neuropathic joint. Additional causes of a hemarthrosis can be seen in Chapter 49 (Arthropathies Associated with Hematologic Diseases, Box 49. In evaluating chronic monoarticular arthritis, what additional studies are indicated in selected patients These additional studies are most helpful in suspected inflammatory etiologies of chronic monoarticular arthritis, as well as those patients without a definitive etiology after initial joint aspiration and radiograph of the affected joint. Are other diagnostic studies useful in the evaluation of chronic monoarticular arthritis Bacterial, fungal, and mycobacterial organisms can be detected with this testing, but not viral organisms. How often is a specific diagnosis made in patients with chronic monoarticular arthritis Appropriate evaluation yields a diagnosis in approximately two-thirds of patients. Fortunately, the most serious and treatable diseases yield to diagnosis if a carefully reasoned clinical approach is taken. The value of synovial fluid assays in the diagnosis of joint disease: a literature survey. History and physical examination, not laboratory testing, are the best tools for diagnosis. Laboratory tests are most useful to confirm the diagnosis based on your history and physical examination. What are the most important tools that the clinician can use on a patient with polyarticular arthritis symptoms Laboratory testing and radiographic or other imaging studies provide definitive answers in only a few instances. Tests are often most useful in confirming the suspected diagnosis or in providing prognostic information. When confronted with a patient with polyarticular symptoms, an inexperienced clinician often will slight the most important, the history and physical examination, opting instead for "shotgun" laboratory testing. No single classification scheme can be used to differentiate the wide variety of diseases presenting with polyarticular symptoms. In most instances, the clinician uses several variables in combination to reduce the number of diagnostic possibilities. Which diseases commonly present with chronic (persisting >6 weeks) polyarticular symptoms Polyarthritis is definite inflammation (swelling, tenderness, warmth) of more than four joints demonstrated by physical examination. A patient with two to four involved joints is said to have pauci- or oligoarticular arthritis. The acute polyarticular diseases (see Question #3) and chronic inflammatory diseases (see Question 4) commonly present with polyarthritis. Polyarthralgia is defined as pain in more than four joints without demonstrable inflammation by physical examination. Diffuse aches and pains are poorly localized symptoms originating in the joints, bones, muscles, or other soft tissues. Describe the three characteristic temporal patterns of joint involvement in polyarthritis. Crystalline arthropathy is the most common category causing this pattern of arthritis. How is the distribution of joint involvement helpful in the differential diagnosis of polyarthritis
The Gower maneuver is abnormal women's health center port st lucie order fosamax australia, and the child will be unable to do a sit-up as a result of weakness menstruation 9 tage buy 70 mg fosamax with visa. The head may hang back as the child is lifted from a lying position, owing to weakness of the neck flexors. The eyelids and face are edematous, and a heliotrope or mauvish rash is noted around the eyes (75%). The most common lung finding is a decreased carbon monoxide diffusing capacity in 50% of patients. Serum muscle enzymes are elevated, but not to the degree seen in the muscular dystrophies. Assays for all muscle-derived enzymes are required (aldolase, creatine kinase, aspartate aminotransferase, and lactate dehydrogenase) because only one may be elevated. In patients who have symptoms such as "classic" skin rash, muscle weakness, and elevated muscle enzymes, the diagnosis can be made clinically. In a child with progressive weakness, other muscle diseases are more likely than polymyositis. Mobility may be impaired because of calcinotic lesions at the joints or as a result of involvement of musculature. It is frequently associated with the metabolic syndrome, insulin resistance, hirsuitism, clitoromegaly, and acanthosis nigricans. Compare the occurrence and frequency of Raynaud phenomenon and Raynaud disease in children and adults. Raynaud phenomenon should be distinguished from normal vasomotor instability, particularly in young girls. It should also be distinguished from acrocyanosis, a rare vasospastic disorder of persistent coldness and bluish discoloration of the hands and feet, which may follow a viral infection. Localized scleroderma may take the form of morphea, with a single patch or multiple patches. Methotrexate is coadministered with the steroids and continued for at least 2 years. Severely painful, migratory polyarthritis with fever (see Chapter 44: Acute Rheumatic Fever and Poststreptococcal Arthritis). Consider immunodeficiency in any child with history of two previous bacterial pneumonias (see Chapter 58: Rheumatologic Manifestations of the Primary Immunodeficiency Syndromes). What bowel disease is most likely to present with arthritis and systemic symptoms Up to 20% of children with Crohn disease have arthritis, which is usually monoarticular or oligoarticular. Children will not volunteer information about their bowel habits, so they must be asked. Furthermore, some children with arthritis due to Crohn disease will not have bowel symptoms or a positive stool guaiac. Leukocytoclastic vasculitis: henoch-schonlein purpura and leukocytoclastic vasculitis. Complete and sustained remission of juvenile dermatomyositis resulting from aggressive treatment. Differences in clinical manifestations between childhood-onset lupus and adult-onset lupus: a metaanalysis. Systemic sclerosis in childhood: clinical and immunologic features of 153 patients in an international database.