Maxalt
"Order maxalt with paypal, advanced pain treatment center edgewood ky".
By: R. Riordian, M.B. B.CH. B.A.O., M.B.B.Ch., Ph.D.
Co-Director, University of Michigan Medical School
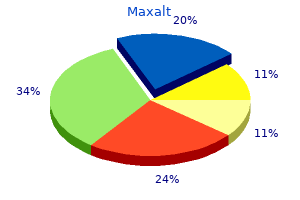
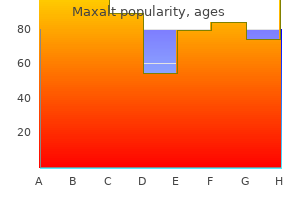
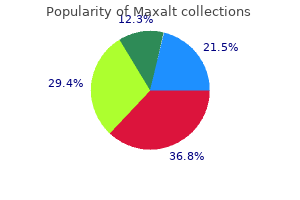
Renal considerations in angiotensin converting enzyme inhibitor therapy: a statement for healthcare professionals from the Council on the Kidney in Cardiovascular Disease and the Council for High Blood Pressure Research of the American Heart Association pain medication for nursing dogs buy genuine maxalt line. Trimethoprim-sulfamethoxazole-induced hyperkalemia in patients receiving inhibitors of the renin-angiotensin system: a population-based study pain solutions treatment center woodstock ga maxalt 10mg. Co-trimoxazole and sudden death in patients receiving inhibitors of renin-angiotensin system: population based study. Meta-analysis of randomized trials of angioedema as an adverse event of Renin-Angiotensin system inhibitors. The path to an angiotensin receptor antagonistneprilysin inhibitor in the treatment of heart failure. Neprilysin Inhibition in Heart Failure with Reduced Ejection Fraction: A Clinical Review. A trial of the beta-blocker bucindolol in patients with advanced chronic heart failure. Comparison of carvedilol and metoprolol on clinical outcomes in patients with 145. Sustained restoration of autonomic balance with long- but not short-acting metoprolol in patients with heart failure. Carvedilol Compared With Metoprolol Succinate in the Treatment and Prognosis of Patients With Stable Chronic Heart Failure: Carvedilol or Metoprolol Evaluation Study. Association of treatment with carvedilol vs metoprolol succinate and mortality in patients with heart failure. Metabolic effects of carvedilol vs metoprolol in patients with type 2 diabetes mellitus and hypertension: a randomized controlled trial. Effects of BetaBlocker Withdrawal in Acute Decompensated Heart Failure: A Systematic Review and Meta-Analysis. An alpha2Cadrenergic receptor polymorphism alters the norepinephrine-lowering effects and therapeutic response of the beta-blocker bucindolol in chronic heart failure. Dysfunctional corin i555(p568) allele is associated with impaired brain natriuretic peptide processing and adverse outcomes in blacks with systolic heart failure: results from the Genetic Risk Assessment in Heart Failure substudy. No therapy studied to date has conclusively been shown to reduce mortality and several may potentially worsen outcomes. Administration as a bolus or continuous infusion appears to be equally efficacious and safe when selected as initial therapy, although high-dose loop diuretic therapy (ie, up to 2. The addition of a thiazide-type diuretic may be considered in patients with diuretic resistance. Such therapy may also be considered in patients who fail to respond to aggressive treatment with diuretics. Vasodilators should be avoided in patients with symptomatic hypotension or reduced left ventricular filling pressure. Vasopressin antagonists such as tolvaptan may be considered in patients with severe euvolemic or hypervolemic hyponatremia. Therapy should only be initiated in a hospital setting to allow for monitoring of volume status and serum sodium concentrations, as rapid correction of serum sodium may result in adverse neurological sequelae. Intravenous inotropes are recommended for maintaining systemic perfusion and end-organ function in hypotensive patients with evidence of severe left ventricular dysfunction and low cardiac output. For those studies that have been published, the heterogeneity of patients enrolled often limits clinical application. Using these three parameters, patients may be classified as low, intermediate, high, and very high risk, with in-hospital mortalities of 2%, 6%, 13%, and 20%, respectively. In addition to guiding therapeutic decision-making, these four hemodynamic profiles are also predictive of clinical outcomes. Compared to dry-warm patients, patients in the wet-warm and wet-cold subsets have a 2-fold and 2. Most patients do not require admission to an intensive care unit and may be admitted to a monitored unit or general medical floor. Patients can become refractory to oral therapies and decompensate after even a relatively mild insult (eg, dietary indiscretion, nonsteroidal anti-inflammatory drug use), medication nonadherence, or concurrent noncardiac illness (eg, infection).
Firstline therapies for volume resuscitation consist of crystalloids such as isotonic saline or balanced solutions pain treatment program johns hopkins discount maxalt on line. Similarly to preventative hydration strategies pain treatment associates west plains mo order 10mg maxalt free shipping, crystalloids such as isotonic saline or balanced solutions are preferred. In addition, the patient should be monitored for body weight changes, fluid intake and urine output, pulmonary and peripheral edema, blood pressure (target mean arterial pressure 65 mm Hg), and serum electrolytes. Stress, inflammation, and injury lead to hypermetabolic/hypercatabolic states and may alter the nutritional requirements. Loss of the normal physiologic and metabolic functions of the kidney and the hypercatabolic response to stress and injury will have a significant impact on the metabolism of nutrients. Derangements in glucose, lipid, and protein metabolism result in hyperglycemia and insulin resistance, hypertriglyceridemia, protein catabolism, and negative nitrogen balance. The latter, in particular, is problematic to manage, as increased amino acid turnover and skeletal muscle breakdown lead to muscle wasting and malnutrition and do not respond well to increasing exogenous protein supplementation. If hemodialysis is carefully monitored and hypotension avoided, better patient outcomes can be achieved. Multiple factors influence decisions to initiate dialysis including specific timing and type of modality. Hemodialysis treatments usually last 3 to 4 hours, with blood flow rates to the dialyzer typically ranging from 200 to 400 mL/min. They differ in the degree of solute and fluid clearance that can be clinically achieved as a result of the use of diffusion, convection, or a combination of both. In direct comparisons of ultrafiltration rates of 25 and 40 mL/kg/h or higher, no difference in mortality has been observed, and there was a tendency toward prolonged need for renal replacement in those who received the higher ultrafiltration rate. Typical anticoagulation is achieved by the administration of parenteral agents such as regional citrate (preferred if increased risk for bleeding is present), unfractionated heparin, low-molecular-weight heparin in some cases, or a direct thrombin inhibitor when other therapies are contraindicated. Infusing fluids after the hemofilter can result in hemoconcentration within the filter, a factor associated with an increased risk of thrombosis of the dialyzer. Replacing fluids before the filter reduces thrombosis risk, but it also reduces solute clearance. The blood circuit in each diagram is represented in red, the hemofilter/dialyzer membrane is yellow, and the ultrafiltration/dialysate compartment is brown. The degree of fluid removal that is accomplished by convection is usually minimal. Although the use of hybrid hemodialysis therapies is increasing, our knowledge of their impact on drug removal is very limited. Excessive sodium intake may override the ability of the diuretics to eliminate sodium. Other clinical states, such as glomerulonephritis, are associated with heavy proteinuria. Intraluminal loop diuretics cannot exert their effect in the loop of Henle if they are extensively bound to proteins present in the urine. Still other patients may have greatly reduced bioavailability of oral furosemide because of intestinal edema, often associated with high preload states, which further reduces oral furosemide absorption. One effective technique to overcome diuretic resistance is to administer loop diuretics via continuous infusion instead of intermittent boluses. Less natriuresis occurs when equal doses of loop diuretics are given as a bolus instead of as a continuous infusion. Furthermore, adverse reactions from loop diuretics (myalgia and hearing loss) occur less frequently in patients receiving continuous infusion compared with those receiving intermittent boluses, ostensibly because higher serum concentrations are avoided. An initial loading dose is recommended prior to the initiation of a continuous infusion of furosemide or its equivalent. With time, these areas of the nephron compensate for the activity of the loop diuretic and increase sodium and chloride resorption. Diuretics that work at the distal convoluted tubule (chlorothiazide and metolazone) or the collecting duct (amiloride, triamterene, and spironolactone) may have a synergistic effect when administered with loop diuretics by blocking the compensatory increase in sodium and chloride resorption95 (see Chapter 49 for more discussion). Of these combinations, oral metolazone is used most frequently because, unlike other thiazides, it produces effective diuresis at a CrCl less than 20 mL/min (0.
Selection of an inotropic drug should also take into account whether patients are receiving chronic -blocker therapy and whether a 1-selective agent (eg wellness and pain treatment center tuscaloosa discount 10mg maxalt, metoprolol succinate) or mixed pain treatment center of franklin tennessee cheap maxalt 10mg line, -blocking agent (eg, carvedilol) is used. Traditionally, milrinone has been advocated in patients who are receiving chronic -blocker therapy because its inotropic effects do not involve -receptor stimulation. In fact, the hemodynamic effects of dobutamine may persist in the presence of -blocker therapy, particularly with 1-selective agents as a result of -receptor upregulation or selective activation of 2-receptors by dobutamine. However, whether this combination provides a therapeutic advantage over the combined use of a positive inotrope and a traditional vasodilator (eg, sodium nitroprusside) is unclear. Regardless of the modality selected, systemic anticoagulation is required to prevent device thrombosis. An Impella device is advanced through the aortic valve, where blood is transferred from the left ventricle to the aorta by an axial flow pump. An inflow cannula is surgically inserted into the apex of the left ventricle, where blood is transferred to an extracorporeal centrifugal flow pump (not shown), where it is returned to the systemic circulation via an outflow cannula surgically inserted into the aorta. Unique features, contraindications, and complications of each type of device will be discussed in the sections to follow. In addition, the devices can cause thrombosis, renal and hepatic dysfunction, and arrhythmias. During counterpulsation, the balloon is synchronized with the electrocardiogram (or alternatively, changes in pressure) so that it inflates during diastole and displaces blood to the proximal aorta, thus increasing diastolic pressure and coronary perfusion. The balloon deflates just prior to the opening of the aortic valve during systole, which causes a sudden "vacuum-like" decrease in aortic pressure, allowing the left ventricle to pump against reduced arterial impedance. It may be particularly useful for patients with myocardial ischemia complicated by cardiogenic shock, although it has not been shown to improve mortality in this setting. Blood is withdrawn from the left atrium by an extracorporeal pump and propelled via an outflow cannula placed percutaneously into a large artery. Due to its placement across the intra-atrial septum, perforation and shunt formation are potential complications with this device. Given the surgical technique required for placement of the CentriMag device, tissue injury is its most common complication. Whereas previous devices provided hemodynamic support via pulsatile flow, newergeneration devices utilize a continuous flow mechanism, allowing them to be smaller in size, less subject to deterioration over time, and conferring an improvement in event-free survival. For complete heart replacement therapy, total artificial heart systems continue to be investigated, although size and embolic complications limit widespread use. Device malfunction may occur with long-term use but has become rare with advances in technology. Suspected pump thrombosis should be promptly evaluated, although no consensus exists on an appropriate treatment strategy (eg, enhanced antiplatelet or anticoagulant therapy, thrombolysis, or pump exchange). Components of this evaluation commonly include past medical, surgical, and psychosocial history, medication and adverse event history, adherence to medications and medical care, comorbid conditions, risks for postoperative complications, and health insurance coverage. Relative contraindications to the use of advanced therapies include excess perioperative risk, irreversible pulmonary hypertension, inability to manage postoperative care (eg, medication therapy, monitoring), and concurrent survival-limiting diseases (eg, malignancy). Another significant percentage of patients are deemed ineligible for heart transplantation because of age, concurrent illnesses, psychosocial factors, or other reasons. The shortage of donor hearts has prompted the development of new surgical strategies, including ventricular aneurysm resection, mitral valve repair, and myocardial cell transplantation, which have resulted in variable degrees of improvement. Foley catheter placement is not recommended unless close monitoring of urine output is not otherwise possible. If relevant, smoking cessation must be addressed to avoid delay in consideration for advanced therapies. Medication changes (initiation, discontinuation, dose change) should be clearly conveyed verbally and in writing and financial coverage for all medication assured. Appropriate follow-up should be scheduled including an appointment at 7-10 days post discharge including a nurse visit or phone call at 3 days for select patients. All patients should be considered for referral to a formal disease management program. In addition, small studies suggest that the inotropic effects of dobutamine may be retained with selectbetablockers. While many of the above parameters may be monitored daily, some will need to be monitored more frequently as dictated by patient clinical status. They may also have pulmonary edema with hypoxemia, respiratory acidosis, and markedly increased work of breathing.
The influence of timing of epinephrine has been described in other analyses and earlier administration appears to be more beneficial than later treatment for elbow pain from weightlifting purchase maxalt master card. In fact gallbladder pain treatment diet 10 mg maxalt amex, some studies have reported increased morbidity with high epinephrine doses, indicative of catecholamine toxicity, including decreased cardiac indices, left ventricular dysfunction, and decreased oxygen consumption and delivery. This discrepancy between animal and human studies could be related to most victims of cardiac arrest having coronary artery disease, which is not encountered in an animal model. Additionally, atherosclerotic plaques (in humans) can aggravate the balance between myocardial oxygen supply and demand and the interval from arrest to treatment is longer in human studies than that encountered in an animal model. Although it acts on various receptors throughout the body, its vasoconstrictive properties are due primarily to its effects on the V1 receptor. First, the metabolic acidosis that frequently accompanies cardiac arrest can blunt the vasoconstrictive effect of adrenergic agents such as epinephrine. Because vasopressin does not act on beta-receptors, this effect does not occur with its use. Vasopressin also may have a beneficial effect on renal blood flow by stimulating V2-receptors in the kidney, causing vasodilation and increased water reabsorption. With regard to splanchnic blood flow, however, vasopressin has a detrimental effect when compared to epinephrine. There was a trend, however, toward a poorer neurologic state or coma among the patients who survived to discharge and received vasopressin. The favorable results observed in the subgroup analysis led to a prospective study evaluating the combination of vasopressin and epinephrine versus epinephrine alone. The time to epinephrine administration may be an important confounding factor for the value of epinephrine during out-of-hospital cardiac arrest. Vasopressin Vasopressin, also known as antidiuretic hormone, is Given the disparate results with epinephrine in published research, it can be considered both a cure and a curse in cardiac arrest. One possible explanation for the negative effects of epinephrine is related to its mechanism of action. Epinephrine causes alphamediated vasoconstriction which increases coronary perfusion but can decrease perfusion to other vital organs. Several studies have compared epinephrine with other adrenergic agonists such as pure alpha-1 agonists (phenylephrine and methoxamine) and agents with more potent alpha-activity (norepinephrine). One potential reason could be the potent alpha-2 effects with epinephrine and the fact that these receptors lie extrajunctionally in the intima of the blood vessels making them more accessible to circulating catecholamines. Thrombolysis Thrombolysis may be considered when cardiac arrest is suspected to be caused by pulmonary embolism. It is reasonable that targeted temperature management be maintained for at least 24 hours after achieving target temperature. Key for evidence-based classifications: Class of recommendations: Class I (Strong). In contrast, a post-hoc subgroup analysis revealed a lower rate of survival (0% vs 5. The utility of a multidrug regimen that also included corticosteroids has been evaluated in the setting of in-hospital cardiac arrest. In a singlecenter trial, patients were randomized to receive either epinephrine alone or 20 units of vasopressin plus 1 mg of epinephrine and 40 mg of methylprednisolone (followed by hydrocortisone in the postresuscitative phase). These favorable results led to a multicenter trial conducted at three centers using the same drug regimen. In lieu of the conflicting results with vasopressin therapy across randomized controlled trials, several meta-analyses have been performed. Subgroup analyses revealed vasopressin may be associated with better outcomes in patients with in-hospital arrests or when used as repeated boluses of four or five times. These results may be confounded by the concomitant use of corticosteroids in some trials. A second meta-analysis included 4,745 patients from six studies (4 out-of-hospital arrest; 2 in-hospital arrest).
If the increase in the Scr is less than 30% from baseline and potassium serum levels are within normal range pain treatment for osteoporosis discount maxalt 10mg otc, the medication can generally be continued hip pain treatment for dogs maxalt 10 mg otc. Simultaneously occurring renal inflammation and microcirculatory dysfunction further amplify these mechanisms. Atheroemboli most commonly develop during vascular procedures that cause atheroma dislodgement, such as angioplasty and 593 aortic manipulations. Thromboemboli may arise from dislodgement of a mural thrombus in the left ventricle of a patient with severe heart failure or from the atria of a patient with atrial fibrillation. Renal artery thrombosis may occur in a similar fashion to coronary thrombosis, in which a thrombus forms in conjunction with an atherosclerotic plaque. However, these small vessels are susceptible to inflammatory processes that lead to microvascular damage and vessel dysfunction when the renal capillaries are affected. Neutrophils invade the vessel wall, causing damage that can include thrombus formation, tissue infarction, and collagen deposition within the vessel structure. Untreated hypertension may also compromise renal microvascular blood flow, causing diffuse renal capillary damage. Drug-induced disease is characterized by renal interstitial dendritic and renal tubular epithelial cells recognition of the offending agent as immunogenic and their activation of T lymphocytes which induce proinflammatory molecules. Once acute interstitial inflammation sets in, it can progress very rapidly to a more destructive fibrogenic process marked by increased interstitial matrix, ischemia, tubular atrophy, and interstitial fibrosis. It serves to filter fluid and solute into the tubules while retaining proteins and other large blood components in the intravascular space. Because the glomerulus is a capillary system, similar damage in the renal vasculature as described above can occur by the same mechanisms. The pathophysiology and specific therapeutic approaches to glomerulonephritis are described in detail in Chapter 47. The remaining 35% are the result of exposure to direct tubule toxins, which can be endogenous (myoglobin, hemoglobin, or uric acid) or exogenous (contrast agents, aminoglycosides, etc. Thus, ischemic conditions caused by severe hypotension or exposure to vasoconstrictive drugs preferentially affect the tubules more than any other portion of the kidney. Further, alterations in cytoskeletal structure lead to a loss of epithelial polarity and barrier function. As a result, the glomerular filtrate starts leaking back into the interstitium and is reabsorbed into the systemic circulation. Additionally, urine flow is obstructed by accumulation of sloughed epithelial cells, cellular debris, and formation of casts. The surviving cells undergo repair, migration, dedifferentiation, and proliferation. Bladder outlet obstruction, the most common cause of obstructive nephropathy, is often the result of a prostatic process (hypertrophy, cancer, or infection), producing a physical impingement on the urethra and thereby preventing the passage of urine. Blockage may also occur at the ureter level secondary to nephrolithiasis, blood clots, sloughed renal papillae, or physical compression by an abdominal process. In these cases, patients have insufficient urine volume to prevent crystal precipitation in the urine. Extremely elevated uric acid concentrations from chemotherapyinduced tumor lysis syndrome can cause obstruction and direct tubular injury as well. It may be a change in urinary character (eg, decreased urine output or urine discoloration), sudden weight gain, or severe abdominal or flank pain. Patients should also be promptly evaluated for any changes in their fluid and electrolyte status. However, there are several limitations associated with its use since it is affected by age, gender, muscle mass, diet, and hydration status. For example, patients with reduced creatinine production, such as those with low muscle mass, may have very low values (less than 0. However, in the presence of improved nutrition and a large muscle mass, a Scr of 1. Assuming a standard daily creatinine production of about 20 mg/kg of lean body weight, one can expect about 1. The most recent Scr reflects the time-averaged kidney function over the preceding time period. Additionally, these equations are complex and are not commonly used in the clinical setting. Urine output measured over a specified period of time (eg, 4-24 hours) allows for short-term assessment of kidney function, but its utility is limited to cases in which it is significantly decreased.