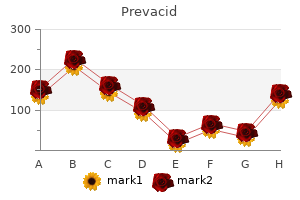
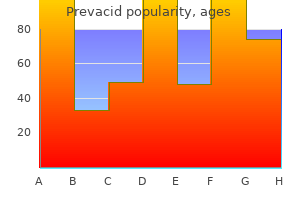
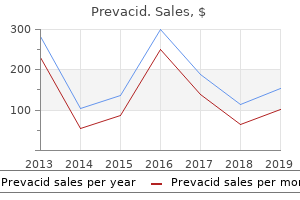
Prevacid
"Cheap prevacid online visa, gastritis diet приват24".
By: S. Cruz, M.B. B.CH. B.A.O., Ph.D.
Clinical Director, University of North Carolina School of Medicine
Ligation of the vein is a plausible surgical option gastritis diet 7 up nutrition effective 15mg prevacid, especially in hemodynamically unstable patients gastritis symptoms medication cheap prevacid 30 mg without prescription,35 however, carries a risk of venous mesenteric ischemia secondary to splanchnic sequestration. Aggressive resuscitation is vital following venous ligation, and a second-look laparotomy is standard. In rare cases, collateral circulation to the descending and sigmoid colons and the upper rectum may be inadequate and result in ischemia; however, this is uncommon because of rich collateral flow. Renovascular injury (renal artery, renal vein, kidney) is suspected when a hematoma is found in zone 2 of the retroperitoneum. Revascularization of renal vessel injury is performed via primary repair, vein patch angioplasty, interposition grafting, or segmental resection with reanastomosis. In cases of bilateral vascular injury, every attempt at revascularization should be made to preserve renal function. Attempts to repair the right renal vein should be made, since the absence of adequate venous collateral flow on the right side will lead to loss of the right kidney. Endovascular approaches to manage mesenteric and renovascular trauma have potential utility, especially in the setting of blunt trauma. Similar to what is seen in other arterial beds, partial-thickness injuries to mesenteric and renal arteries may result in intimal defects or pseudoaneurysms detected on axial imaging. These can be managed with endovascular stents to prevent ischemia or delayed rupture, though observation and serial imaging may be most appropriate in some cases. Hematoma or hemorrhage in the portal triad is suggestive of portal vein and/or hepatic artery injury. Though some portal vein injuries may be repaired without extensive surgical exposure, a right medial visceral rotation may be required. These patients present in such poor condition that complex reconstructions are rarely feasible or advisable. Complex reconstructions should only be done in patients with associated hepatic artery injury that is not amenable to repair, as combined absence of blood flow through the portal vein and hepatic artery will lead to liver failure and death. Ligation is another option that should be considered for devastating retropancreatic injuries, as long as hepatic artery flow can be preserved. The internal branch gives off multiple branches to pelvic structures, while the external branch proceeds under the inguinal ligament and into the leg to become the femoral artery. Injury to the iliac arteries often leads to the development of a pelvic, zone 3, hematoma. The iliac arteries are among the most commonly injured vascular structures in the abdomen. The proximity and shared course of the iliac veins make combined arteriovenous injuries a frequent occurrence. The ascending colon can be reflected medially and superiorly via right medial visceral rotation, exposing the pelvic retroperitoneum. Reconstruction can also be accomplished with end-to-end anastomosis of autogenous saphenous vein or prosthetic grafts. Iliac injuries are amenable to bailout or damage-control procedures when a patient is critically ill due to other traumatic injuries. Temporary shunt insertion, arterial ligation with delayed extra-anatomical reconstruction, or packing of venous injury may be employed in this situation. Iliac vein injury can be even more complex with regard to gaining access and control of the vessel. Occasionally, the iliac artery must be divided to allow adequate access to the venous structures, and then reconstructed following venous repair. Concerns of edema and compartment syndrome following prolonged ischemic time or vein ligation merit a low threshold for lower-extremity fasciotomies. Endovascular techniques have shown utility in selected cases of iliac artery injury. In a recent analysis of the National Trauma Data Bank from 2002 to 2008, the proportion of patients with common/external iliac artery injuries undergoing endovascular repair increased from 0. By comparison, the proportion for thoracic aortic injury, where endovascular treatment may be preferred, increased from 0.

Keywords erythromelalgia; erythralgia; erythroprosopalgia; acromelalgia; Weir-Mitchell disease; Mitchell disease Definition and historical perspective Erythromelalgia is a rare condition of the extremities characterized by the triad of redness gastritis symptoms blood discount 15mg prevacid amex, warmth chronic gastritis metaplasia order genuine prevacid on-line, and pain. The symptom complex of intermittent acral warmth, pain, and erythema that defines erythromelalgia has been well documented in the medical literature for more than 150 years. The term erythromelalgia was coined in 1878 by Mitchell2 from erythros (red), melos (extremity), and algos (pain); some have since referred to it as Mitchell disease. As we discover more about the link between a vasculopathy and neuropathy in this syndrome, it seems that Mitchell was prophetically accurate when he entitled the original manuscript "On a Rare Vasomotor Neurosis of the Extremities. Although many authors agree that erythermalgia is perhaps more accurate, erythromelalgia is the term most commonly used, and it is the term used in this chapter. Although the condition is mysterious, it is not as mysterious as was once believed. Related names used by some include Weir-Mitchell disease, Mitchell disease, and acromelalgia. They used the term erythermalgia to describe idiopathic conditions or conditions due to other diseases that are unresponsive to aspirin therapy. An unwieldy term, erythermomelalgia, accounts for the four cardinal symptoms and signs of the condition, but it is not in general use. Weir Mitchell2,8 applied the three inclusion criteria used in the original description of the syndrome: red, hot, and painful extremities. Brown17 added three additional criteria in 1932: induction and exacerbation of symptoms by warming, relief by cooling, and unresponsiveness to therapy. Minor criteria were typical precipitating factors (heat exposure, effort), typical relieving factors (cold, rest), elevated skin temperature in affected skin, and response of symptoms to acetylsalicylic acid. It is secondary when symptoms are caused by a primary disease such as a hemorrheological, metabolic, connective tissue, musculoskeletal, or infectious disease; are induced by drugs; or are part of a paraneoplastic phenomenon. Classification of erythromelalgia into primary and secondary types may be controversial when comorbid conditions are mislabeled as underlying diseases that cause erythromelalgia. Classification of incomplete forms of erythromelalgia is also controversial; for example, some patients report that their feet are blue when symptoms are present. The problem with all definitions is that each criterion depends on clinical subjective judgment. The diagnosis of erythromelalgia is based on history because there are no objective physical findings. Clinical presentation the essential elements of this clinical syndrome, as described by its name, are intermittent (occasionally continuous) redness of an acral area. Common terms used to describe the pain include "piercing," "burning," and "discomfort. During an episode, they try to cool their feet in many ways, sometimes resorting to extraordinary measures to alleviate the pain, such as putting their feet in ice or walking barefoot in snow. In the largest reported series (168 patients), symptoms predominantly involved feet (148 patients, 88. In the majority of patients, symptoms are intermittent; episodes, precipitated by specific triggers, can last from minutes to hours. In a minority of patients, erythromelalgia symptoms are continuous, although they may wax and wane. Patients with continuous symptoms usually report that their symptoms started intermittently and then became more frequent and prolonged until they were continuous. In the series of 168 patients,8 symptoms were intermittent in 163 patients (97%) and continuous in 5 (3%). The specific precipitant for erythromelalgia varies from person to person, but the most frequent precipitant is an increase in temperature of the affected acral area. This may be caused by an increase in ambient temperature, and patients may experience increases in severity and frequency of attacks during the summer.
Neck vascular trauma Mechanism and Anatomic Considerations With respect to penetrating injuries to the neck chronic gastritis natural remedies prevacid 15mg mastercard, hemodynamic instability or the presence of hard signs of vascular injury mandate emergent operative exploration prior to detailed axial imaging gastritis cancer order prevacid 30mg line. In the stable patient, anatomic considerations have traditionally played an important role in determining who should proceed to surgery, based on the anatomic "zones" of the neck, and who should get further diagnostic imaging. When a penetrating injury does not violate the platysma muscle, the risk of occult, deeper injury requiring operative repair is low and therefore no immediate operative exploration is warranted. However, if the platysma is violated, surgical management has traditionally been dictated by which zone of the neck is affected. A modification of this system describes the uppermost extent of zone I as the cricoid cartilage. In stable patients, the anatomic zone of injury does not guide decision-making, and additional diagnostic imaging is commonly pursued. These are generally based on injury mechanism and may include (1) concomitant displaced mid-face fracture, (2) basilar skull fracture/petrous bone fracture, (3) diffuse axonal injury/Glasgow Coma Scale 8, (4) cervical spine fracture, and/or (5) clothesline type injury or near-hanging. More proximal injuries may require sternotomy for vascular control whereas more distal injuries may be very difficult to access and, in fact, may be preferentially treated with an endovascular approach. Primary repair of injuries can be performed in some cases, but for extensive injuries or complete transection, interposition grafting with great saphenous vein is usually preferred. Temporary intravascular shunts can be placed in patients who must be further resuscitated and/or have other injuries addressed prior to definitive repair. In rare instances, ligation is performed to prevent exsanguination or if vascular damage is irreparable. Vertebral artery injuries can be difficult to access surgically and are uncommonly repaired with complex surgical reconstruction techniques. Surgeons are more likely to perform proximal ligation or endovascular embolization/occlusion for control of hemorrhage, relying on collateral posterior circulation to prevent cerebral ischemia. Artery transection with extravasation (grade V) should prompt urgent intervention, whether it be open or endovascular. The acceptance of endovascular techniques in the management of these injuries has increased, particularly because many are difficult to access surgically. Systematic reviews of patients with blunt or penetrating carotid injury have demonstrated good technical success rates with acceptable perioperative morbidity and promising short-term patency (80% up to 2 years) of carotid stent grafts. Venous bleeding can be temporized with direct pressure while repair of concomitant injuries is performed. In the setting of troublesome hemorrhage, the brachiocephalic, internal jugular, or subclavian veins can be ligated with relative impunity. If primary repair can be accomplished without compromising more than 50% of the injured vessel, a lateral venorrhaphy is appropriate. Repair/reconstruction should always be attempted in the presence of obvious venous hypertension or for one of the brachiocephalic or internal jugular veins if bilateral injury is present. Thoracic vascular trauma Mechanism and Anatomic Considerations Penetrating wounds to the thorax have the potential to injure the heart, great vessels, pulmonary vessels, and descending thoracic aorta, in which case exsanguinating hemorrhage can rapidly lead to death. It is typically not possible to determine which structures may have been damaged simply by examining the entry and/or exit wounds. The cardiac "box" overlies the precordium and is bounded by the nipple lines laterally, the clavicles superiorly, and the inferior costal margin inferiorly. When penetrating injuries to the box are discovered, it is assumed that trauma to the heart and other mediastinal structures has occurred until proven otherwise. Blunt injury to the thorax has potentially catastrophic consequences, with aortic injury and cardiac injury among the most common and fatal. Motor vehicle collisions are the most common mechanism and lead to deceleration and crush injuries. Often, patients will have multiple rib and/or clavicular fractures as evidence of the massive forces involved. It must be kept in mind that some patients may have no external manifestations of injury in the thorax. Hemorrhage into the chest cavity (whether by blunt or penetrating mechanism) leads to hemothorax, which is initially managed with a tube thoracostomy. Massive hemothorax requires urgent thoracotomy for surgical management of ongoing hemorrhage. The primary views obtained are pericardial, hepatorenal, perisplenic, and suprapubic (pelvic) views. In addition, a thoracic view can be obtained to evaluate for pneumothorax and/or hemothorax.
The diagnosis can be made by measuring compartment pressures at the point of exertional pain in affected individuals gastritis symptoms lap band order prevacid 15 mg with mastercard. Compartment pressures are normally elevated following exercise but return to normal within 3 minutes gastritis diet beans cheap prevacid online visa. The majority of patients with temporal arteritis are encompassed in which of the following groups What is the optimal initial treatment for subacute upper extremity ischemia caused by temporal arteritis Which of the following is of greatest benefit in the treatment of patients with Buerger disease Extensive vascular calcification in a young patient with normal parathyroid function suggests which of the following Abdominal coarctation is most frequently discovered during evaluation for which symptom Calf claudication in a nonsmoker younger than 30 years is most commonly caused by which disorder The early objective diagnosis of anterior compartment syndrome is best made by which finding Compartment pressure measurement with Wick or the "solid-state transducer in catheter " monitor 10. Usually associated with an abnormal relationship between the popliteal artery and the lateral head of gastrocnemius muscle b. Predisposes affected individuals to anterior collateral ligament injury Bibliography Espinosa G, Font J, Tassies D, et al. Cooling augments alpha-2-adrenoceptormediated contractions in the rat tail artery Am J Physiol. The different photoplethsymographic patterns can help to distinguish patients with primary and sclerodermic Raynaud phenomenon. Cold provocation testing and hand-arm vibration syndrome-an audit of the results of the Department of Trade and Industry scheme for the evaluation of miners. Intravenous iloprost infusion in patients with Raynaud phenomenon secondary to systemic sclerosis. Long-term experience of bosentan for treating ulcers and healed ulcers in systemic sclerosis patients. Long term effects of thoracic sympathectomy on microcirculation in the hands of patients with primary Raynaud disease. A systematic review of the outcomes of digital sympathectomy for the treatment of chronic digital ischemia. Fat grafting to the hand in patients with Raynaud phenomenon: a novel therapeutic modality Plastic Reconst Surg. Incidence and natural history of Raynaud phenomenon: a long-term follow-up (14 years) of a random sample from the general population. Permanent visual loss and cerebrovascular accidents in giant cell arteritis: predictors and response to treatment. Clinical presentation and vascular imaging in giant cell arteritis of the femoropopliteal and tibioperoneal arteries. Giant cell arteritis with low erythrocyte sedimentation rate: frequency of occurrence in a population-based study Arthritis Rheum. Erythrocyte sedimentation rate and Creactive protein in the evaluation of disease activity and severity in polymyalgia rheumatica: a prospective follow-up study Semin Arthritis Rheum. How does previous corticosteroid treatment affect the biopsy findings in giant cell (temporal) arteritis Efficacy of unilateral versus bilateral temporal artery biopsies for the diagnosis of giant cell arteritis. Treatment of giant cell arteritis using induction therapy with high-dose glucocorticoids, a double-blind, placebo controlled randomized prospective trial. Combined treatment of giant-cell arteritis with methotrexate and prednisone: a randomized, double blind, placebo- controlled trial. Infliximab for maintenance of glucocortcosteroid-induced remission fo giant cell arteritis: a randomized trial. A double-blind placebo controlled trial of etanercept in patients with giant cell arteritis and corticosteroid side effects.