Unisom
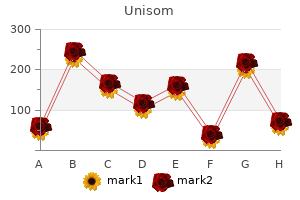
"Cheap unisom 25 mg with amex, insomnia quick fix".
By: D. Amul, M.B. B.CH. B.A.O., Ph.D.
Deputy Director, San Juan Bautista School of Medicine
During treatment with insulin and fluids insomnia games ashland ky unisom 25 mg without a prescription, various factors contribute to the development of hypokalemia insomnia yify subtitles discount 25mg unisom visa. These include insulinmediated potassium transport into cells, resolution of the acidosis (which also promotes potassium entry into cells), and urinary loss of potassium salts of organic acids. The results of most clinical trials do not support the routine use of bicarbonate replacement, and one study in children found that bicarbonate use was associated with an increased risk of cerebral edema. The etiology of and optimal therapy for cerebral edema are not well established, but overreplacement of free water should be avoided. During illness or when oral intake is compromised, patients should (1) frequently measure the capillary blood glucose; (2) measure urinary ketones when the serum glucose is >16. The physical examination reflects profound dehydration and hyperosmolality and reveals hypotension, tachycardia, and altered mental status. It is also possible that the liver is less capable of ketone body synthesis or that the insulin/glucagon ratio does not favor ketogenesis. A small anion gap metabolic acidosis may be present secondary to increased lactic acid. In patients taking diuretics, the potassium deficit can be quite large and may be accompanied by magnesium deficiency. The patient should be discharged from the hospital on insulin, though some patients can later switch to oral glucoselowering agents. Chronic complications can be divided into vascular and nonvascular complications (Table 19-7). Nonvascular complications include problems such as gastroparesis, infections, and skin changes. The risk of chronic complications increases as a function of the duration of hyperglycemia; they usually become apparent in the second decade of hyperglycemia. Many of these patients have glycemic control that is indistinguishable from those who develop microvascular complications, suggesting that there is a genetic susceptibility for developing particular complications. These events correlate with fasting and postprandial plasma glucose levels as well as with the A1C. Other factors (dyslipidemia and hypertension) also play important roles in macrovascular complications. Nonenzymatic glycosylation results from the interaction of glucose with amino groups on proteins. A second theory is based on the observation that hyperglycemia increases glucose metabolism via the sorbitol pathway. Intracellular glucose is predominantly metabolized by phosphorylation and subsequent glycolysis, but when increased, some glucose is converted to sorbitol by the enzyme aldose reductase. Increased sorbitol concentration alters redox potential, increases cellular osmolality, generates reactive oxygen species, and likely leads to other types of cellular dysfunction. However, testing of this theory in humans, using aldose reductase inhibitors, has not demonstrated significant beneficial effects on clinical endpoints of retinopathy, neuropathy, or nephropathy. A fourth theory proposes that hyperglycemia increases the flux through the hexosamine pathway, which generates fructose-6-phosphate, a substrate for O-linked glycosylation and proteoglycan production. A possible unifying mechanism is that hyperglycemia leads to increased production of reactive oxygen species or superoxide in the mitochondria; these compounds may activate all four of the pathways described above. Individuals in the intensive diabetes management group received multiple administrations of insulin each day along with extensive educational, psychological, and medical support. Individuals in the conventional diabetes management group received twice-daily insulin injections and quarterly nutritional, educational, and clinical evaluation. Individuals in the intensive diabetes management group achieved a substantially lower hemoglobin A1C (7. There was a nonsignificant trend in reduction of macrovascular events during the trial (most individuals were young and had a low risk of cardiovascular disease). For example, individuals in the intensive diabetes management group for a mean of 6.
Somatotropin: Growth hormone; a 191-amino acid polypeptide hormone that is synthesized and secreted from the somatotroph cells of the anterior pituitary insomnia new haven discount unisom 25mg with mastercard. It acts primarily on hepatocytes sleep aid dosage order 25mg unisom visa, although muscle and adipose cells also have receptors for growth hormone. A potent stimulator of growth hormone release is ghrelin, a polypeptide hormone secreted by the stomach that acts directly on somatotrophs. In general, many environmental factors including stress, exercise, nutrition, and sleep influence circulating levels of growth hormone. The overall effect is a pulsatile pattern of growth hormone release reaching a maximum in children and young adults shortly after the onset of deep sleep. Levels of growth hormone fluctuate dramatically and are suppressed in normal individuals after oral glucose administration. Growth hormone plays a major role in cell proliferation and in regulating protein, lipid, and carbohydrate metabolism. It stimulates protein synthesis and the accompanying amino acid uptake in many tissues. In adipocytes, it increases fat utilization by stimulating triglyceride breakdown and oxidation. It opposes effects of insulin by suppressing its ability to stimulate glucose uptake and by stimulating gluconeogenesis. Interestingly, injection of growth hormone stimulates insulin secretion, leading to hyperinsulinemia. Growth hormone acts directly by binding its receptors in the plasma membrane of target cells to influence cell proliferation and metabolism. In this case, tyrosine kinase activity resides on the same polypeptide as hormone-binding activity. Normal proliferation of somatic cells requires both thyroid hormone and growth hormone. The profound physiologic role of growth hormone is revealed by conditions resulting from either its deficiency or excess. By contrast, excessive secretion leads to giantism, if expressed before the growth plates have closed, or acromegaly, if overproduction is initiated in the adult. Usually, growth hormone overproduction in the adult is the result of a noncancerous pituitary tumor. Overgrowth (thickening) of bones and connective tissues leads to the characteristic features of acromegaly, with accompanying enlargement of other tissues including the heart. In appearance she had unusually coarse features; a noticeable enlargement of the tongue, hands, and feet; and a deep voice. Although not pregnant or nursing, she unexpectedly began producing breast milk (galactorrhea). Which one of the following possibilities is most likely to explain all of these symptoms Which one of the following metabolic alterations is most likely to be observed after beginning this treatment Growth hormone opposes insulin action resulting in decreased glucose utilization and symptoms of diabetes mellitus. Excessive bone and tissue growth lead to the characteristic coarse facial features, enlarged tongue and heart, bone thickening, and other characteristics associated with this syndrome. The most common cause of growth hormone overproduction in the adult is a noncancerous pituitary tumor. The patient is concerned about having thyroid problems because her friend has similar symptoms and was diagnosed with hyperthyroidism. Once in puberty, a woman usually has fairly regular menstrual cycles as dictated by the estrogen and progesterone secretion of the ovaries until about age 40 to 50 years. During a period of 2 to 4 years, some women may experience irregular menses because of irregular ovulation until finally there are no further menses. Definitions Apoptosis: Programmed cell death that leads to the destruction of cells leaving membrane-bound particles that are shed or taken up by phagocytosis. When binding to receptors on the plasma membrane of the granulose cells of the ovarian follicle, it stimulates the synthesis and secretion of estradiol. It binds to receptors on the thecal cells of the ovarian follicle to increase synthesis of androgens. When binding to receptors on the corpus luteum, it increases the synthesis of progesterone.
He has had diabetes since the age of 12 and has always required insulin for therapy insomnia 08 electro remix buy unisom without prescription. He insomnia quote fight club buy unisom uk, however, notes that his morning fasting blood sugar is high without taking any carbohydrates. His physician describes the morning high sugars as a result of biochemical processes in response to the nighttime hypoglycemia. What are the biochemical processes that govern the response to the nighttime hypoglycemia Biochemical mechanism of hypoglycemia: the low nighttime serum blood sugar stimulates the counter-regulatory hormones to try to raise the glucose level. These include epinephrine, glucagon, cortisol, and growth hormone, which affect the glucose level and raise it by the time morning comes around. The danger is that if nighttime blood glucose levels are not measured, the physician may interpret the patient as having hyperglycemia and require even higher doses of insulin. This would be exactly the wrong treatment, since the hypoglycemia is leading to counter-regulatory hormone reaction, and a very low sugar level bound to the high level in the morning. Definitions Epinephrine: Adrenaline; a catecholamine hormone derived from the amino acids phenylalanine or tyrosine that is synthesized and secreted by the adrenal medulla in response to stress. Ketoacidosis: An elevation of the ketone body concentration that decreases the pH of the arterial blood to a pathologic condition. Acetoacetate and -hydroxybutyrate are formed by liver enzymes that condense molecules of acetyl-CoA, thus regenerating CoA for continual use in -oxidation of fatty acids. Ketone bodies are exported from the liver and can be used by some extrahepatic tissues for energy generation. Protein phosphatase 1: An enzyme that will hydrolyze phosphate groups from target proteins such as glycogen synthase, phosphorylase, phosphorylase kinase, and the phosphorylated form of inhibitor 1. The phosphorylated inhibitor 1 is a substrate that binds well but is hydrolyzed slowly. While bound to protein phosphatase 1, the phosphorylated inhibitor 1 serves as an inhibitor of the enzyme. During periods of increased glucose availability, the liver increases uptake, storage, and utilization of glucose. The latter is hydrolyzed to free glucose by glucose-6-phosphatase, the enzyme unique to gluconeogenic tissues, such as the liver. Although found within the cytosol of virtually every cell, glycogen is primarily concentrated in muscle (cardiac and skeletal) and liver. Schematic diagram showing the events that lead to the export of glucose from the liver cell during times of low blood glucose. During the latter period of time, glycogen will be mobilized as a readily available source of glucose. In the case of muscle, glycogen is used selfishly, as an energy source by the myocyte only. In contrast, liver glycogen will be mobilized to help maintain blood glucose levels. As glycogenesis is the reciprocal pathway to glycogenolysis, gluconeogenesis is the reciprocal pathway to glycolysis. Glycolysis, the "lysis" of glucose to two pyruvate molecules, is a ubiquitous metabolic pathway, whereas gluconeogenesis occurs in only a select number of tissues, including the liver. During periods of increased glucose availability, flux through the glycolytic pathway increases, thereby utilizing this readily available fuel source. In contrast, during periods of decreased glucose availability, rates of gluconeogenesis increase, in an attempt to maintain blood glucose levels. The sources of carbon for gluconeogenesis depend on the given metabolic situation. Gluconeogenesis is an energetically demanding process, which is driven by the -oxidation of fatty acids. When the rate of acetyl-CoA generation through fatty acid -oxidation exceeds the rate of acetyl-CoA oxidation via the Krebs cycle and oxidative phosphorylation (ox phos), acetyl-CoA accumulates. The biochemical pathways of the synthesis of glycogen (glycogenesis) and its breakdown to glucose 6-phosphate (glycogenolysis). Schematic diagram of the interplay of fatty acid breakdown and ketone body formation with the synthesis (gluconeogenesis) and degradation of glucose (glycolysis).

There are many subtypes that are based on the presenting histology; however sleep aid that works unisom 25 mg otc, a papillary presentation should raise suspicion for papillary carcinoma sleep aid doxylamine purchase unisom without a prescription. Oxyphil describes the eosinophilic granular cytoplasm resulting from increased numbers of mitochondria in the neoplastic cells. Benign follicular adenomas can present with endocrine atypia, which refers to the presence of nuclear pleomorphism, and atypia. Because a well-differentiated follicular carcinoma can be relatively unremarkable, it is essential to look for invasion of the capsule or blood vessels to determine malignancy. The pathology report from a fine needle aspiration of the nodule describes a follicular neoplasm, the differential of which includes a benign follicular adenoma and a malignant follicular carcinoma. Which is the single best histologic criterion to differentiate between these two neoplasms Hyperplasia of follicles Inspissation of colloid Invasion into vessels Number of mitoses Presence of atypia [16. Physical examination finds enlargement of the thyroid gland resulting from the presence of several small masses in both thyroid lobes. These nodules are surgically resected, and the pathology report from this surgical specimen diagnoses a papillary carcinoma. Which of the following histologic changes is most characteristic of this type of carcinoma The lesion is removed surgically, and histologic sections reveal groups of poorly differentiated tumors cells within a stroma with large areas of amyloid. This familial form of this type of malignancy is associated with abnormalities of which of the following protooncogenes The differential diagnosis of a cold nodule of the thyroid includes follicular adenoma, follicular carcinoma, papillary carcinoma, medullary carcinoma, and anaplastic carcinoma. The only histologic means to differentiate between these two neoplasms is the presence of cells invading through the capsule surrounding the tumor or into blood vessels. The most common histologic type of thyroid carcinoma is called a papillary carcinoma. This type of malignancy, which has the best prognosis among thyroid carcinomas, may be solitary or multifocal. The term papillary refers to the finger-like projections formed by fronds of tumor cells with fibrovascular cores. The papillary areas sometimes are associated with the formation of concentric calcified structures called psammoma bodies. The presence of these papillary projections is not necessary for the diagnosis of papillary thyroid carcinoma. Instead, the definitive diagnosis is based on characteristic nuclear features, which include ground glass nuclei ("Orphan Annie eyes"), nuclear grooves, and intranuclear inclusions (cytoplasmic invaginations into the nucleus). Medullary carcinoma of the thyroid is a malignant neoplasm that originates from the parafollicular C cells of the thyroid. Stromal aggregates of procalcitonin are seen histologically within these tumors as amyloid, which is a type of protein that demonstrates an "apple-green" birefringence with a special Congo red stain. Although most cases of medullary thyroid carcinomas are sporadic, the familial form is associated with abnormalities of the ret protooncogene. This type of malignancy also is seen in multiple endocrine neoplasia types 2 and 3. The most common thyroid carcinoma is papillary carcinoma, which affects people of all ages. Treatment in each case is surgical except for anaplastic carcinoma, in which external radiation therapy is used. The physical examination reveals tenderness and induration of the left temporal region. Other confirmatory studies: the gold standard is a temporal artery biopsy of at least 2 to 3 cm in length. Typically, the symptoms of temporal arteritis occur in a patient aged 50 years or older with sudden-onset headache over the temporal region, disturbances in vision, and polymyalgia rheumatica; these findings warrant immediate treatment. Polymyalgia rheumatica includes the symptoms of joint pain, morning stiffness, and muscle ache. Inflammation of the temporal artery increases the likelihood of thrombosis of the ophthalmic artery, causing irreversible blindness. Consequently, if temporal arteritis is suspected clinically, corticosteroids are administered immediately, with a subsequent temporal biopsy to establish the diagnosis.

