Clozaril
"Buy clozaril 25mg low price, medicine zofran".
By: E. Ugolf, M.S., Ph.D.
Program Director, Joan C. Edwards School of Medicine at Marshall University
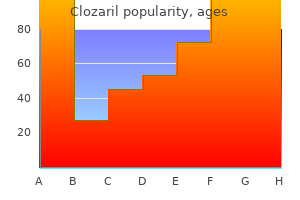
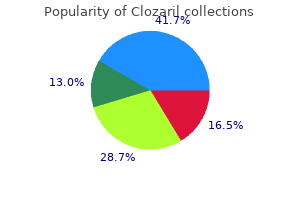
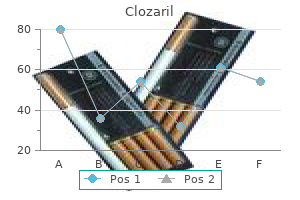
Reynolds and associates (2013) reported higher rates of cardiovascular disease and all-cause mortality in 37 medications derived from plants buy 50mg clozaril with amex,709 adult offspring of overweight and obese mothers medicine reaction buy clozaril 100mg on line. Similar cardiometabolic health effects in offspring were echoed by Gaillard and colleagues (2016). Other data support that excessive maternal weight gain in pregnancy may predict obesity in adult offspring (Lawrence, 2014; Reynolds, 2010). Last, rates of glucose intolerance and metabolic syndrome are higher among offspring of obese women (Gaillard, 2016; Tan, 2015). But such studies raise the possibility of fetal programming, that is, the fetal environment may lead to adverse adult health outcomes. Elucidation is limited by insufficient data on potential maternal and genetic predisposing factors and on the environment of the infant and child in relation to diet and activity. The science of epigenetics has provided some support for the possibility that perturbations of the maternalfetal environment can adversely alter postdelivery events (Kitsiou-Tzeli, 2017). Also possible are contributions of the maternal-child environment subsequent to birth (Gluck, 2009). These and other factors regarding fetal programming are discussed in Chapter 44 (p. Intuitively, maternal weight must increase sufficiently to provide for fetal and placental tissue accrual and for amnionic fluid and maternal blood volume expansion. The American College of Obstetricians and Gynecologists (2015) endorses these Institute guidelines. However, these recommendations were issued without firm scientific evidence to support them, and their value remains unproven (Rasmussen, 2010). For example, recent studies differ with respect to the effect of insufficient weight gain for obese women. Bodnar and colleagues (2016) reported no greater risk for lowbirthweight or small-for-gestational-age newborns among 47,494 obese women who had inadequate weight gain during pregnancy. Bogaerts and associates (2015) found that even weight loss among obese women did not yield poor fetal growth. In contrast, however, Hannaford and coworkers (2017) reported that obese women who gained less than the Institute recommendations were almost three times more likely to deliver a small-for-gestational-age neonate. Another study similarly found an almost twofold greater risk among obese women who lost weight during pregnancy (Cox Bauer, 2016). Apart from inadequate weight gain, excessive gestational weight gain may portend greater risks for the obese mother. Berggren and coworkers (2016) noted that overweight and obese women accrued maternal fat rather than lean mass with excessive gestational weight gain. From another analysis, overall higher rates of hypertensive disorders, cesarean delivery, and fetal overgrowth as well as lower rates of spontaneous preterm birth and fetal undergrowth were found among women gaining more than recommended (Johnson, 2013). During pregnancy, overweight and obese women gain more weight than recommended compared with normal-weight gravidas (Endres, 2015). Moreover, overweight and obese women have excessive postpartum weight retention at 1 year, and one third retain at least 20 pounds more than their prepregnancy weight. Dietary Intervention Several dietary interventions can help limit and achieve the weight-gain targets listed in the previous section. In one randomized trial of exercise in 300 overweight women, risks for gestational diabetes were lowered (Wang, 2017). That said, in another trial, 75 overweight women were randomly assigned to routine care or to a 16-week moderate-intensity stationary cycling program starting after midpregnancy. Also, a Cochrane database analysis of 11,444 women suggests that lifestyle interventions confer only a modest reduction in maternal weight gain, and their benefits for fetal overgrowth, cesarean delivery rate, and adverse neonatal outcome are not significant (Muktabhant, 2015). Regarding neonatal outcomes, the poor success of lifestyle interventions during pregnancy has been attributed to their late introduction, that is, after early gene expression within the placenta has already been programmed (Catalano, 2015). Prenatal Care Close prenatal monitoring detects most early signs of diabetes or hypertension.
If it does not soon subside or if deep-vein involvement is suspected medications bad for liver discount clozaril online amex, appropriate diagnostic measures are performed treatment definition discount clozaril online. Superficial vein thrombosis raises the risk of deep-vein thrombosis four- to sixfold. Superficial thrombophlebitis is typically seen in association with varicosities or as a sequela of an indwelling intravenous catheter. According to Marik and Plante (2008), 70 percent of gravidas presenting with a pulmonary embolism have associated clinical evidence of deep-vein thrombosis. And recall that between 30 and 60 percent of women with a deep-vein thrombosis will have a coexisting silent pulmonary embolism. Clinical Presentation In almost 2500 nonpregnant patients with a proven pulmonary embolism, symptoms included dyspnea in 82 percent, chest pain in 49 percent, cough in 20 percent, syncope in 14 percent, and hemoptysis in 7 percent (Goldhaber, 1999). Other predominant clinical findings typically include tachypnea, apprehension, and tachycardia. In some cases, an accentuated pulmonic closure sound, rales, and/or friction rub is heard. Right axis deviation and T-wave inversion in the anterior chest leads may be evident on the electrocardiogram. In others, nonspecific findings may include atelectasis, an infiltrate, cardiomegaly, or an effusion (Pollack, 2011). Vascular markings in the lung region supplied by the obstructed artery can be lost. Although most women are hypoxemic, a normal arterial blood gas analysis does not exclude pulmonary embolism. Thus, the alveolar-arterial oxygen tension difference is a more useful indicator of disease. More than 86 percent of patients with acute pulmonary embolism will have an alveolar-arterial difference >20 mm Hg (Lockwood, 2012). Even with massive pulmonary embolism, signs, symptoms, and laboratory data to support the diagnosis may be deceptively nonspecific. Massive Pulmonary Embolism this is defined as embolism causing hemodynamic instability (Tapson, 2008). Acute mechanical obstruction of the pulmonary vasculature causes increased vascular resistance and pulmonary hypertension followed by acute right ventricular dilation. In otherwise healthy patients, significant pulmonary hypertension does not develop until 60 to 75 percent of the pulmonary vascular tree is occluded (Guyton, 1954). These are suspected when the pulmonary artery pressure is substantively increased as estimated by echocardiography. Note that the crosssectional area of the pulmonary trunk and the combined pulmonary arteries is 9 cm2. A large saddle embolism could occlude 50 to 90 percent of the pulmonary tree, causing hemodynamic instability. As the arteries give off distal branches, the total surface area rapidly increases, that is, 13 cm2 for the combined five lobar arteries, 36 cm2 for the combined 19 segmental arteries, and more than 800 cm2 for the total 65 subsegmental arterial branches. It is important in these cases to infuse crystalloids carefully and to support blood pressure with vasopressors. As discussed on page 1018, oxygen treatment, endotracheal intubation, and mechanical ventilation are completed preparatory to thrombolysis, filter placement, or embolectomy (Tapson, 2008). Diagnosis In most cases, recognition of a pulmonary embolism requires a high index of suspicion that prompts objective evaluation. Exposure of the mother and fetus to ionizing radiation is a concern when investigating a suspected pulmonary embolism during pregnancy. However, this concern is largely overruled by the hazards of missing a potentially fatal diagnosis. Moveover, erroneously assigning a diagnosis of pulmonary embolism to a pregnant woman is also fraught with problems. It unnecessarily exposes the mother and fetus to the risks of anticoagulation treatment and will impact delivery plans, future contraception, and thromboprophylaxis during subsequent pregnancies. Therefore, investigations should aim at diagnostic certainty (Konstantinides, 2014). There is enhancement of the pulmonary artery with a large thrombus on the right (arrow) consistent with pulmonary embolism.
Logically 340b medications purchase clozaril 100mg visa, antibodies directed against this glycoprotein would reverse its anticoagulant activity and promote thrombosis medicine hat news purchase clozaril once a day. This is important from an obstetrical viewpoint because 2-glycoprotein I is expressed in high concentrations on the syncytiotrophoblast surface. Complement activation may contribute to its pathogenesis (Avalos, 2009; Tsokos, 2011). Teleologically, this seems appropriate because the decidua intuitively should be a critical area to prevent coagulation that might lead to intervillous space thrombosis. Another possibility is that 2-glycoprotein I may be involved in implantation, and this glycoprotein may result in pregnancy loss via an inflammatory mechanism (Iwasawa, 2012; Meroni, 2011). This antibody group induces prolongation in vitro of the prothrombin, partial thromboplastin, and Russell viper venom times. Thus, paradoxically, this so-called anticoagulant is actually powerfully thrombotic in vivo. Antibodies against Natural Anticoagulants Some antiphospholipid antibodies are also directed against the natural anticoagulant proteins C and S (Robertson, 2006). Another is directed against the anticoagulant protein annexin V, which is expressed in high concentrations by syncytiotrophoblast (Giannakopoulos, 2013). Testing for these other antibodies is not recommended (American College of Obstetricians and Gynecologists, 2017). In one study, treatment of women with these nonconventional antibodies offered some benefits, such as a lower pregnancy loss rate (Mekinian, 2016). First, one of two clinical criteria-which are vascular thrombosis or certain pregnancy morbidity-must be present. The diagnosis can be further stratified based on the number of these tests that are positive (Miyakis, 2006). Some Clinical Features of Antiphospholipid Syndrome Venous thrombosis-thromboembolism, thrombophlebitis, livedo reticularis Arterial thrombosis-stroke, transient ischemic attack, Libman-Sacks cardiac vegetations, myocardial ischemia, distal extremity and visceral thrombosis and gangrene Hematological-thrombocytopenia, autoimmune hemolytic anemia Other-neurological manifestations, migraine headaches, epilepsy; renal artery, vein, or glomerular thrombosis; arthritis and arthralgia Pregnancy-preeclampsia syndrome, recurrent miscarriage, preterm delivery, fetal-growth restriction, fetal death Data from Giannakopoulos, 2013; Moutsopoulos, 2015. The partial thromboplastin time is generally prolonged because the anticoagulant interferes with conversion of prothrombin to thrombin in vitro. Tests considered more specific are the dilute Russell viper venom test and the platelet neutralization procedure. Branch and Khamashta (2003) recommend conservative interpretation of results based on repeated tests from a reliable laboratory that are consistent with each clinical case. Pregnancy and Antiphospholipid Antibodies As noted, nonspecific low levels of antiphospholipid antibodies are identified in approximately 5 percent of normal adults (Branch, 2010). When Lockwood and coworkers (1989) first studied 737 normal pregnant women, they reported that 0. Subsequent investigations confirmed this, and taken together, they totaled almost 4000 normal pregnancies with an average prevalence for antiphospholipid antibodies of 4. This is similar to that for normal nonpregnant individuals (Harris, 1991; Yasuda, 1995). Pregnancy Pathophysiology It is not precisely known how antiphospholipid antibodies cause damage, but it is likely that their actions are multifactorial. Platelets may be damaged directly by antiphospholipid antibody or indirectly by binding 2-glycoprotein I, which causes platelets to be susceptible to aggregation (Giannakopoulos, 2013). One theory proposes that phospholipid-containing endothelial cell or syncytiotrophoblast membranes may be damaged directly by the antiphospholipid antibody or indirectly by antibody binding to either 2-glycoprotein I or annexin V (Rand, 1997, 1998). This prevents the cell membranes from protecting the syncytiotrophoblast and endothelium. This exposes the basement membrane, to which damaged platelets can adhere and form a thrombus. Pierro and associates (1999) reported that antiphospholipid antibodies decreased decidual production of the vasodilating prostaglandin E2. Diminished protein C or S activity and greater prothrombin activation may also be contributory (Zangari, 1997). Finally, uncontrolled placental complement activation by antiphospholipid antibodies may play a role in fetal loss and growth restriction (Holers, 2002).
Cabergoline is generally considered safe for use in pregnancy (Araujo treatment 20 nail dystrophy buy online clozaril, 2015; Auriemma medicine lake buy generic clozaril 100mg, 2013). Lebbe and colleagues (2010) described 100 pregnancies exposed to cabergoline and found no adverse effects. Note the layering of complex fluid within the mass, which was found during surgery to be hemorrhage. In normal pregnancy, pituitary growth hormone levels decrease as placental epitopes are secreted. Fewer than 100 cases of acromegaly have been reported during pregnancy (Cheng, 2012; Dias, 2013; Motivala, 2011). Pregnancy is probably rare in women with acromegaly because half are hyperprolactinemic and anovulatory. During pregnancy, affected women are at marginally greater risk for gestational diabetes and hypertension (Caron, 2010; Dias, 2013). Management is similar to that for prolactinomas, with close monitoring for symptoms of tumor enlargement. And, transsphenoidal resection, generally considered first-line treatment outside of pregnancy, may be necessary for symptomatic tumor enlargement during pregnancy (Motivala, 2011). Guven and associates (2006) reported a case of pituitary apoplexy necessitating emergent transsphenoidal adenoma resection and cesarean delivery at 34 weeks. Diabetes Insipidus the vasopressin deficiency evident in diabetes insipidus is usually due to agenesis or destruction of the neurophypophysis (Robertson, 2015). Most women require increased doses during pregnancy because of an increased metabolic clearance rate stimulated by placental vasopressinase (Lindheimer, 1994). By this same mechanism, subclinical diabetes insipidus may become symptomatic or cases of transient diabetes insipidus may be encountered during pregnancy (Bellastella, 2012; Robertson, 2015). The prevalence of vasopressinase-induced diabetes insipidus is estimated at 2 to 4 per 100,000 pregnancies (Wallia, 2013). This probably is due to altered vasopressinase clearance because of hepatic dysfunction. Sheehan Syndrome Sheehan (1937) reported that pituitary ischemia and necrosis associated with obstetrical blood loss could result in hypopituitarism. With modern methods of hemorrhagic shock treatment, Sheehan syndrome is now seldom encountered (Feinberg, 2005; Pappachan, 2015; Robalo, 2012). Affected women may have persistent hypotension, tachycardia, hypoglycemia, and lactation failure. Because deficiencies of some or all pituitary-responsive hormones may develop after the initial insult, Sheehan syndrome can be heterogenous and may not be identified for years (Tessnow, 2010). In one cohort study of 60 women from Costa Rica with Sheehan syndrome, the average time to diagnosis was 13 years (Gei-Guardia, 2011). Because adrenal insufficiency is the most life-threatening complication, adrenal function should be immediately assessed in any woman suspected of having Sheehan syndrome. After glucocorticoid replacement, subsequent analyses and replacement of thyroid, gonadal, and growth hormones is considered. Lymphocytic Hypophysitis this rare autoimmune pituitary disorder is characterized by massive infiltration by lymphocytes and plasma cells with parenchymal destruction of the gland. Many cases are temporally linked to pregnancy (Foyouzi, 2011; Honegger, 2015; Melmed, 2015). There are varying degrees of hypopituitarism or symptoms of mass effect, including headaches and visual field defects. A mass accompanied by a modestly elevated serum prolactin level-usually <100 pg/mL-suggests lymphocytic hypophysitis. The etiology is unknown, but nearly 30 percent have a history of coexisting autoimmune diseases including Hashimoto thyroiditis, Addison disease, type 1 diabetes, or pernicious anemia. The disease may be self-limited, and a careful withdrawal of hormone replacement is attempted after inflammation subsides (Foyouzi, 2011; Melmed, 2015). Thyroid 20(10):1175, 2010 Abalovich M, Gutierrez S, Alcaraz G, et al: Overt and subclinical hypothyroidism complicating pregnancy. Thyroid 12(1):63, 2002 Abbassi-Ghanavati M, Casey B, Spong C, et al: Pregnancy outcomes in women with thyroid peroxidase antibodies. Obstet Gynecol 116(2, Pt 1):381, 2010 Abdelmannan D, Aron D: Adrenal disorders in pregnancy. Accessed January 7, 2017 American College of Obstetricians and Gynecologists: Thyroid disease in pregnancy.
Breast reconstruction treatment 7th march bournemouth purchase clozaril 100 mg with amex, if desired symptoms copd buy generic clozaril 50mg line, is typically delayed until after delivery (Viswanathan, 2011). That said, Caragacianu and coworkers (2016) described good results in 10 pregnant women who underwent immediate reconstruction after mastectomy. Chemotherapy is usually given with both positive- and negative-node breast cancers. In premenopausal women, survival rates with this approach are improved, even if lymph nodes are cancer free. For node-positive disease, multiagent chemotherapy is begun if delivery is not anticipated within several weeks. If an anthracycline-based agent such as doxorubicin is used, pretherapy maternal echocardiography is performed because of associated cardiotoxicity (Brewer, 2011). The effects of pregnancy on the course of breast cancer and its prognosis are complex. Breast cancer is more aggressive in younger women, but whether it is more aggressive during pregnancy in these same women is debatable (Azim, 2014). Clinically, most studies indicate little difference in overall survival rates with pregnancy-associated breast cancer compared with similarly aged and staged nonpregnant women (Beadle, 2009). Other reports note worse overall survival rates with pregnancy-associated breast cancer (Rodriguez, 2008). These investigators do conclude, however, that later disease stages are more prevalent in pregnant women. Indeed, breast cancer is usually found at a more advanced stage in pregnant women, and thus overall prognosis is diminished (Andersson, 2015). The aggregate of studies published after 1990 indicate that up to 60 percent of pregnant women have concomitant axillary node involvement at diagnosis. And although, stage for stage, the 5-year survival rate is comparable in pregnant and nonpregnant women, the more advanced stages that are typical of pregnant women worsen their prognosis (Kuo, 2017; Zemlickis, 1992). Pregnancy Following Breast Cancer After breast cancer treatment, chemotherapy will render some women infertile, and options for childbearing are limited (Kim, 2011). For those who become pregnant, long-term maternal survival rates are not adversely affected (Averette, 1999; Velentgas, 1999). One metaanalysis of 10 studies found that for women with early breast cancer, pregnancy that occurs 10 months after diagnosis may, in fact, confer a survival benefit (Valachis, 2010). Because recurrences are more common soon after treatment, it seems reasonable to delay conception for 2 to 3 years. Hormonal contraceptive methods are contraindicated, and a copper-containing intrauterine device is an excellent longacting reversible method for many. That said, women who conceive do not appear to have diminished survival rates (Ives, 2006). Notably, women treated with tamoxifen are at risk for several months after its discontinuation to have a newborn with congenital anomalies. This drug has an extremely long half-life, and thus delaying conception is recommended for at least 2 months after tamoxifen completion (Braems, 2011). Fine-needle aspiration is indicated for a suspicious nodule (Alexander, 2017; Gharib, 2016). Thus, delayed surgical treatment does not usually alter outcome (Yazbeck, 2012; Yu, 2016). In some types of thyroid cancer, radioiodine is used for primary or postoperative treatment. First, transplacental 131I is avidly trapped by the fetal thyroid gland to cause hypothyroidism. Second, during lactation, the breast also concentrates a substantial amount of iodide. This may pose neonatal risk due to radioiodine- contaminated milk ingestion and maternal risk from significant breast irradiation. To limit maternal exposure, a delay of 3 months between lactation and thyroid ablation will more reliably ensure complete breast involution (Sisson, 2011). In women with thyroid cancer who ultimately receive 131I doses, pregnancy should be avoided for 6 months to 1 year.

