Sildalist
"Buy sildalist 120mg cheap, why smoking causes erectile dysfunction".
By: C. Asam, M.B.A., M.B.B.S., M.H.S.
Clinical Director, Kaiser Permanente School of Medicine
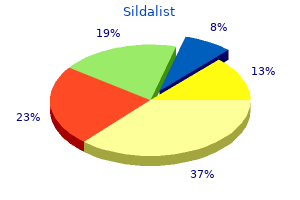
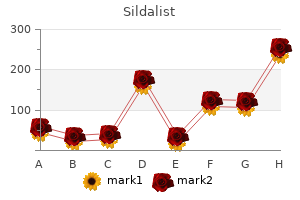
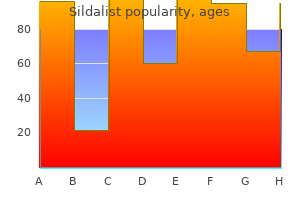
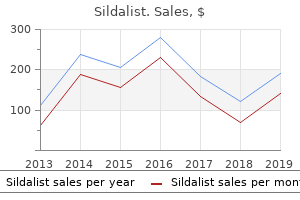
In general larger and more proximal stones are less likely to pass spontaneously erectile dysfunction medication non prescription 120mg sildalist visa, even with medical expulsive therapy erectile dysfunction doctor new jersey order genuine sildalist on-line, and are often an indicator for earlier intervention. The approach to stone removal depends on its size, location, and composition, as well as on urinary tract anatomy. The major options for ureteral stone removal include percutaneous nephrolithotomy and extracorporeal shock wave lithotripsy; open surgical extraction is rarely required. Percutaneous nephrolithotomy involves the passage of a flexible scope through the kidney and into the urinary space. Extracorporeal shock wave lithotripsy focuses external sound waves onto the kidney stone, thereby causing it to fragment into smaller stones that can more easily be passed spontaneously. Meta-analyses suggest that percutaneous nephrolithotomy is the treatment of choice for the majority of ureteral stones, A8 A9 because it results in longer stone-free rates and a lower need for retreatment, even though it is associated with more complications, usually minor, and a longer hospitalization compared with shock wave lithotripsy. As a result, every patient who forms an initial stone should undergo evaluation with the goal of preventing recurrent stones. The history should focus on uncovering factors that predispose to stone formation. All stones should be analyzed to assist in defining the underlying metabolic abnormality and to guide therapy. Many stone formers are erroneously instructed to eliminate all calcium from their diet, a practice that not only increases stone formation but also may induce bone demineralization. Sodium intake should be estimated because sodium excretion obligates calcium excretion, thereby potentially leading to urinary supersaturation. Excessive animal protein intake increases metabolic acid production, which increases bone demineralization and calciuria. Hypercalcemic disorders-including malignancy (Chapter 232), hyperparathyroidism (Chapter 232), and sarcoidosis (Chapter 89)-often result in hypercalciuria, increased urinary supersaturation, and calcium stone formation. Malabsorptive gastrointestinal disorders, such as Crohn disease (Chapter 132) and celiac disease (Chapter 131), or weight reduction surgery (Chapter 207), such as ileal resection or jejunoileal bypass, will often result in calcium oxalate stone formation from increased oxalate absorption and excretion as well as volume depletion. Medications that can cause calcium stone formation include loop diuretics, which increase urinary calcium excretion, as well as salicylates and probenecid, which increase urinary uric acid excretion. Various medications that can themselves precipitate into stones include intravenous acyclovir, high-dose sulfadiazine, triamterene, and the antiretroviral agents indinavir and nelfinavir. Other medications that inhibit renal tubular carbonic anhydrase activity, such as acetazolamide and topiramate, can lead to metabolic acidosis, bone resorption, hypercalciuria, lower urinary citrate excretion, and higher urinary pH, all of which promote the formation of calcium phosphate stones. Stones that develop at a young age suggest a genetic disorder, such as primary hyperoxaluria or cystinuria. Basic laboratory testing should include levels of serum electrolytes (sodium, potassium, chloride, and bicarbonate), creatinine, calcium, phosphorus, uric acid, 25-hydroxyvitamin D, and thyroid-stimulating hormone. If the serum calcium is above and the serum phosphorus is below the midrange of normal, a serum parathyroid hormone level should be obtained. An elevated urine pH combined with bacteriuria (Chapter 268) suggests struvite stones. Because urease production may stimulate struvite stone formation despite low bacterial colony counts, the laboratory must identify all bacteria and determine antibiotic sensitivities even with low colony counts. If no bacteria are isolated, cultures for Ureaplasma urealyticum should be requested. In patients with recurrent stones and/or high-risk characteristics for recurrence, a 24-hour urine collection can determine the levels of calcium, oxalate, citrate, sodium, urate, phosphorus, and creatinine, as well as the calculation of supersaturation with respect to calcium oxalate, calcium phosphate, and uric acid (Table 117-1). An elevated supersaturation should lead the clinician to determine the individual components of the urine that are causing the increased supersaturation, and efforts can then be made to rectify these abnormalities. Cystine should also be measured at least once in every stone former to exclude cystinuria and regularly in patients who form cystine stones. Multivitamins should be discontinued about 5 days before the collection to prevent any antioxidant effect on the urine sample. Dairy products are preferred over calcium supplements because clinical studies indicate that women taking supplemental vitamin D and calcium have a significant increase in stone formation. Potassium citrate (10 to 40 mEq/day)15 will increase urinary citrate excretion, bind urinary calcium, and further decrease recurrent stone formation. A 24-hour urine collection can be repeated in a month or two to assess the response to therapy. Patients with diet-related hyperoxaluria should be instructed to limit or avoid foods with high oxalate content such as cocoa, nuts, tea, and green leafy vegetables such as spinach. Because dietary calcium and oxalate bind in the gut, patients should consume these foods with calcium-containing foods.
Similarly erectile dysfunction pills at cvs 120 mg sildalist otc, if keto acids are completely cleared into the urine erectile dysfunction 27 generic 120mg sildalist amex, ketoacidosis may be manifested as a hyperchloremic acidosis rather than as an anion gap acidosis. A2 In general, the correction of metabolic acidemia should be based on a calculated amount, with not more than 50% of the estimate given before recalculation. Hypokalemia may accompany distal renal tubular acidosis and may improve with treatment. Citrate should be avoided as an alkalinizing salt in patients with low glomerular filtration rate. Proximal renal tubular acidosis in children may affect growth and require large quantities of bicarbonate in excess of 1 to 2 mEq/kg per day to correct the acidosis because ingested alkali is promptly excreted in alkaline urine. In adults, treatment is often deferred because the steady-state acidosis allows a normal acid excretion rate. In type 4 renal tubular acidosis, treatment of hyperkalemia with a lowpotassium diet, thiazide, or loop diuretics or sodium polystyrene sulfonate often improves urinary acidification without the use of bicarbonate salts. The urinary anion, or charge, gap helps distinguish renal tubular acidosis from extrarenal bicarbonate loss. In renal diseases such as distal renal tubular acidosis, however, the urinary anion gap will be zero or positive because of either the failure of ammoniagenesis or the excretion of sodium plus potassium with bicarbonate. In children, disorders such as medullary cystic kidney disease (Chapter 118) and cystinosis (Chapter 119) usually result in renal failure by the teenage years. These patients are candidates for renal replacement therapy, including transplantation. Chronic metabolic acidosis in children, if not well treated, is associated with rickets (Chapter 231) and short stature. In response to increased systemic pH, alveolar ventilation is decreased to increase Pco2 and thereby decrease pH. However, respiratory compensation is generally less effective in cases of metabolic alkalosis than in cases of metabolic acidosis. A second mechanism that may blunt respiratory compensation is intracellular acidosis in the brain in the setting of hypokalemia. The result is that the ventilatory response to metabolic alkalosis is highly varied: many patients with metabolic alkalosis maintain nearly normal Pco2 levels, and the level rarely rises above 60 mm Hg. Extracellular volume depletion stimulates the renin-angiotensin-aldosterone pathway, and high aldosterone levels superimposed on increased distal urinary flow rates result in increased K+ excretion and hypokalemia. Important but rare genetic syndromes characterized by urinary chloride wasting include Bartter syndrome and Gitelman syndrome. Bartter syndrome is an autosomal recessive salt-losing state associated with extracellular volume depletion and excessive urinary chloride loss that results in hypokalemia and hypochloremic metabolic alkalosis. Secondary increases of plasma renin and aldosterone occur, as does renal juxtaglomerular cell hyperplasia. Because calcium reabsorption occurs in the thick ascending limb of Henle, Bartter syndrome (Chapter 119), like furosemide, causes hypercalciuria and nephrocalcinosis as well as polyuria due to decreased urinary concentrating ability. Gitelman syndrome is an autosomal recessive cause of extracellular volume depletion, urinary chloride wasting, and hypokalemic metabolic alkalosis. Urinary concentrating ability is preserved, and patients are hypocalciuric because decreased NaCl reabsorption in the distal tubule is associated with a decrease in calcium excretion. These effects reduce renal Na+ loss but at the expense of maintaining the metabolic alkalosis. Significant K+ losses, which occur as a result of the bicarbonaturia and hyperaldosteronism, lead to hypokalemia, which is actually due to renal, not gastrointestinal, losses as a consequence of attempts to maintain extracellular volume. The patient may be hypovolemic, hypokalemic, and alkalemic, but because Na+, K+, and acid-base balance are intrinsically linked, lifethreatening volume depletion, potassium depletion, and alkalemia are usually avoided. Most nonrenal metabolic alkaloses with volume depletion are due to gastrointestinal losses. The sweat gland, like the principal cell in the kidney, contains the aldosteronesensitive epithelial sodium channel, so Na+ absorption from the glandular duct renders the lumen electronegative. When Cl- absorption is decreased in cystic fibrosis (Chapter 83), the lumen becomes more negative, thereby decreasing Na+, Cl-, and fluid absorption and also leading to salty sweat; the proportionally large Cl- loss generates a hypochloremic metabolic alkalosis. Metabolic Alkalosis of Renal Origin with Volume Expansion and Hypertension the renal conditions that cause metabolic alkalosis and volume expansion are due to a proportionately greater increase in Na+ reabsorption above what is required to maintain a steady state of Na+ balance, rather than primary loss of the Cl- anion. At first, the alkalosis is mild, but increased cortical collecting duct Na+ reabsorption will also lead to increased K+ secretion and hypokalemia.
Heparin and heparin sulfate proteoglycans are naturally present on endothelial cells erectile dysfunction doctor in jacksonville fl generic sildalist 120 mg line, so antithrombin inactivation of thrombin and other coagulation proteases most likely occurs physiologically on vascular surfaces rather than in fluid plasma erectile dysfunction vacuum pumps pros cons buy generic sildalist. Thrombin itself is the activator of protein C, and this reaction occurs rapidly only on the surfaces of intact vascular endothelial cells, where thrombin A thorough history is paramount in evaluating a patient for a possible systemic bleeding disorder. In addition to asking the patient about spontaneous bleeding episodes in the past, the responses to specific hemostatic challenges should be recorded. A bleeding tendency may be suspected if a patient previously experienced excessive hemorrhage after surgery or trauma, including common events such as circumcision, tonsillectomy, labor and delivery, menses, dental procedures, vaccinations, and injections. Conversely, a history of normal blood clotting after such specific challenges in the recent past is just as important to note. It may be a better test of the integrity of systemic hemostasis than any laboratory measurement can provide. In a patient with a history of excessive or unexplained bleeding, the initial goal is to determine whether the cause is a systemic coagulopathy or localized anatomic or mechanical problem with a blood vessel. This situation is encountered most frequently in patients with excessive postoperative bleeding, which could be due to either local surgical trauma or a coagulation abnormality, or both. A history of prior bleeding suggests a coagulopathy, as does the finding of bleeding from multiple sites. Even diffuse bleeding may arise from anatomic rather than hemostatic abnormalities. An example of this is recurrent mucosal hemorrhage in patients with hereditary hemorrhagic telangiectasia (Chapter 164). Conversely, a single episode of bleeding from an isolated site may be the initial manifestation of a coagulopathy. The history must include a survey of coexisting systemic diseases and drug ingestions that could affect hemostasis. Other drugs, such as antibiotics, also may be associated with a bleeding tendency by causing abnormal platelet function or thrombocytopenia. Although a positive history provides an important clue to a possible inherited coagulopathy, a negative history does not exclude a familial cause; for example, 20% of patients with classic hemophilia have a completely negative family history of bleeding. Mild bleeding events are commonly reported by patients with and without subsequently laboratory-documented bleeding disorders, sometimes making it difficult for hematologists to define a "significant bleeding history. More precise quantification of bleeding symptoms is being attempted by using "bleeding score" instruments such as the Vicenza bleeding score to help discriminate, in conjunction with laboratory testing, between healthy subjects and those with mild bleeding disorders. Patterns of clinical bleeding, as revealed by the history and physical examination, may be characteristic of certain types of coagulopathy (Table 162-1). These may involve petechiae, which are pinpoint cutaneous hemorrhages that appear particularly over dependent extremities (characteristic of severe thrombocytopenia), ecchymoses (common bruises), purpura, gastrointestinal and genitourinary tract bleeding, epistaxis, and hemoptysis. In these types of disorders, bleeding tends to occur spontaneously or immediately after trauma. In contrast, patients with inherited or acquired coagulation factor deficiencies, such as hemophilia, or those on anticoagulant therapy tend to bleed from deeper tissue sites. It should be suspected whenever a very low platelet count is unexpectedly reported in a patient who does not exhibit any clinical bleeding. Examination of the blood smear can also reveal clues to the cause of real thrombocytopenia, such as fragmented red blood cells in thrombotic thrombocytopenic purpura. It measures the time to cessation of bleeding after a standardized incision over the volar aspect of the forearm. However, the test is prone to problems related to quality control, reproducibility, sensitivity, and specificity.

In patients with acquired aplastic anemia erectile dysfunction herbs order sildalist visa, this complication likely evolves through a process of clonal selection and adaptation and for that reason is seen less commonly in patients completely responsive to treatment than in those with less than complete responses (who therefore have ongoing suppression of hematopoiesis) impotence pump buy sildalist with a mastercard. This suggests that more effective strategies of immunosuppressive therapy may better control ongoing marrow damage and decrease the incidence of clonal evolution. Stem cell transplantation with nonmyeloablative approaches has the potential of curing the marrow failure component of these diseases and prolonging life. However, it does nothing to reduce the other common life-threatening complication of squamous cell carcinoma. There are good theoretical reasons for anticipating that successful transplantation will reduce the likelihood of clonal evolution to myelodysplasia and acute leukemia. The decision to transplant is influenced by other key factors, as described earlier. In light of these complexities no clear-cut "when-to-transplant" rule can be applied to all patients with these diseases, but it is generally accepted that transplantation early in childhood is associated with fewer short- and long-term complications. Taking these difficult issues into account, all patients should be evaluated early in an experienced transplantation center, and family members should be screened by hematologists, geneticists, and genetic counselors with use of specialty laboratories. In patients with dyskeratosis, small case series report good outcomes after fludarabine-containing nonmyeloablative conditioning regimens, but studies of sufficient size are not available to permit concrete recommendations except that patients should be referred to an experienced center in light of the other organ systems uniquely at risk. In children with Fanconi anemia, with proper conditioning regimens, matched sibling donor transplant recipients have expected 5-year survival rates of 90% or more, and with modern conditioning regimens alternative donor transplants, in children 10 years of age or younger, are equally successful. In patients with Diamond-Blackfan anemia, sibling donor transplant recipients have 3-year survival rates of about 80%, but the role of matched unrelated donor transplants has not been established. For patients with acquired aplastic anemia, small molecules that selectively target the T-cell clones responsible for hematopoietic suppression and enhance the activity of regulatory T-cells19 may provide more effective and less toxic strategies for immunosuppressive therapy. For all patients with aplastic anemia, further improvements in alternative donor transplantation have made this modality more widely available for patients who had not been previously considered to be optimal candidates. For children with non-severe aplastic anemia, the 10-year progression-free survival rate is only about 25%, suggesting that prospective trials of early intervention. For patients with inherited bone marrow failure syndromes, the Future Treatments genes for which have been largely identified, the possibility of stem cell gene therapy holds enormous theoretical promise and has been validated in murine models of the disease and by experiments of nature. Horse versus rabbit antithymocyte globulin in immunosuppressive therapy of treatment-naive aplastic anemia: a systematic review and meta-analysis. A landscape of germ line mutations in a cohort of inherited bone marrow failure patients. Current knowledge and priorities for future research in late effects after hematopoietic cell transplantation for inherited bone marrow failure syndromes: consensus statement from the Second Pediatric Blood and Marrow Transplant Consortium International Conference on Late Effects after Pediatric Hematopoietic Cell Transplantation. Late effects screening guidelines after hematopoietic cell transplantation for inherited bone marrow failure syndromes: consensus statement from the Second 16. In a patient with pancytopenia, which of the following abnormalities in the peripheral blood smear would provide a useful indicator that the cause of the pancytopenia is aplastic anemia None of the above Answer: E the peripheral blood smear in aplastic anemia is generally normal, even in severe cases. This does not mean that the peripheral blood smear does not provide useful information about the etiology of pancytopenia in many cases. For example, hypersegmented polymorphonuclear leukocytes (A) suggest megaloblastic anemia (which in more advanced stages can cause pancytopenia, not just anemia). Nucleated (B) and teardrop-shaped (C) red cells suggest a "myelophthisic" process that involves invasion of the bone marrow by "foreign" elements (like metastatic cancer, fibrosis, or granulomas). The pathogenesis of most cases of acquired aplastic anemia can be attributed to: A. Radiation exposure Answer: D Environmental exposure to myelosuppressive chemicals and radiation are now uncommon causes of aplastic anemia. The majority of patients with acquired aplastic anemia have an autoimmune disease characterized by oligoclonal T-cell populations that function to repress stem cell function. This accounts for the favorable responses to immunosuppressive therapy in such patients. A 19-year-old man with severe aplastic anemia is diagnosed by chromosomal breakage testing to have Fanconi anemia. Bone marrow transplant from a matched related donor after fludarabinebased conditioning C. Cord blood hematopoietic stem cell transplant after conditioning that includes irradiation D.

