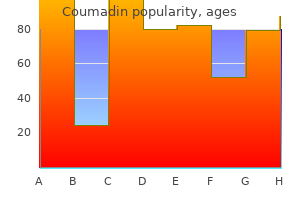
Coumadin
"Buy cheap coumadin 5 mg on-line, blood pressure medication over the counter".
By: V. Khabir, M.B. B.A.O., M.B.B.Ch., Ph.D.
Clinical Director, California University of Science and Medicine
Apical ligament this joins the apex of the dens to the anterior margin of the foramen magnum heart attack marlie grace generic 2mg coumadin otc, and is a fibrous remnant of the notochord (an invaginated rod of cells during embryological development that is located between ectoderm and endoderm) arteria jugularis buy coumadin 1mg with visa. They include the radioscapholunate (ligament of Testut), radial collateral, radiocapitate and volar radiotriquetral ligaments. Alar ligaments the alar ligaments lie obliquely on either side of the apical ligament. Its origin is from the medial border of the distal radius and it inserts in to the base of the ulnar styloid. Shoulder joint Transverse humeral ligament Part of the joint capsule that bridges the gap between greater and lesser tubercles of humerus. Glenohumeral ligaments Three thickened bands between the humerus and labrum, which reinforce the anterior part of shoulder, joint capsule. Coracohumeral ligament this is a strong ligament that runs from the coracoid process to the front of the greater tubercle of humerus. They serve as a window through which the retinacular ligament passes and act to retain different parts of integument in position. The subscapular and its dorsal branch the circumflex scapular artery from the third part of the axillary artery. This arterial anastomosis provides a collateral circulation in case of obstruction of the subclavian artery. There are various sites of anastomosis including the infraspinous fossa, medial border of the scapula, surgical neck of the humerus, thoracic walls and acromion. The smaller anterior circumflex humeral artery passes laterally, deep to coracobrachialis and biceps. The larger posterior circumflex humeral artery passes medially through the posterior wall of the axilla in the quadrangular space with the axillary nerve. The fibres extend between the web spaces of the digits and lie immediately beneath the skin to help create the web space. It begins at the lateral border of the first rib and ends at the inferior border of teres major to become the brachial artery. It is divided in to three parts by pectoralis minor: First part: between the lateral border of the first rib and the medial border of pectoralis minor One branch: superior thoracic artery Second part: lies posterior to pectoralis minor Two branches: thoracoacromial artery, lateral thoracic artery Third part: lateral border of pectoralis minor to the inferior border teres major Three branches: subscapular artery, anterior circumflex humeral artery, posterior circumflex humeral artery. Anterior oblique ligament this is a primary stabilizer of the trapeziometacarpal joint and is taut in abduction, extension and pronation. It originates from the tuberosity of the trapezium and inserts on the volar ulnar edge of the thumb metacarpal base. It originates from the metacarpal head and inserts in to the medial aspect and the base of the proximal phalanx of the thumb. All are synovial joints except the cuboidonavicular joint, which is a fibrous joint. Brachial artery this begins as a continuation of the axillary artery at the lower border of teres major and ends just distal to the elbow joint, dividing in to radial and ulnar arteries. In the proximal arm the brachial artery lies medially but spirals laterally to take up a position midway between both epicondyles of the humerus. It is crossed obliquely from lateral to medial by the median nerve in the mid arm. Medial and posterior to the artery is the ulnar nerve, which leaves it in the lower part of Arteries of the upper limb Scapular anastomosis the dorsal scapular, suprascapular and descending branch of the superficial cervical artery arise from the first part of the 564 Chapter 24: Anatomy oral core topics the arm to pass through the medial intermuscular septum. The artery can be exposed in the groove at the medial border of biceps between biceps and triceps. Profunda brachii Muscular Nutrient to the humerus Superior ulnar collateral Inferior ulnar collateral: divides in to anterior and posterior branches. It ends as it passes through the adductor hiatus in the adductor magnus to become the popliteal artery. It emerges from under the inguinal ligament with the femoral vein medial to it, both within the femoral sheath. As the artery enters the adductor canal it lies on adductor longus then adductor magnus. Four branches arise from the artery in the femoral triangle: Superficial epigastric artery Superficial circumflex iliac artery Superficial external pudendal artery Deep external pudendal artery. The profunda femoris artery is the main branch of the femoral artery, and is given off posterolaterally just below the femoral sheath.
Composition and structure Neurovascular supply the blood supply to tendons is derived primarily through the musculotendinous junction arteria lusoria definition purchase coumadin 5 mg online, with some further communication with the periosteal vessels at the insertion In those tendons with a paratenon hypertension updates 2014 purchase 5 mg coumadin fast delivery, blood vessels penetrate the tendon throughout its length In those tendons with a synovial sheath, the outer and inner sheaths (parietal and visceral, respectively) are linked by a mesotenon, which transmits the vessels. The mesotenon may be continuous, or it may be confined to vinculae, as in the long flexors of the digits Further nutrition is derived from the synovial fluid, and this may be the major source of nutrition for some long tendons, such as the long flexors of the fingers the blood vessels form a network in the epitenon and then pass between fascicles in the endotenon the nerve supply is derived from the corresponding muscle, and tendons contain both fast and slow adapting sensory organs (Golgi organs, Pacinian corpuscles and Ruffini endings). Mechanical behaviour Tendons are viscoelastic structures and, like all viscoelastic structures, they display creep, hysteresis and stress relaxation. In tendons with a synovial sheath there is controversy over the relative contributions from two healing processes: Intrinsic: cell invasion occurs from the tendon ends and from the epitenon Extrinsic: healing occurs via granulation tissue that invades via the tendon sheath. Extrinsic healing is more likely to produce adhesions and lead to a less satisfactory clinical outcome. Ligaments Ligament structure is generally similar to that of tendons although there are some differences. Ligaments tend to be strongest when forces are applied parallel to their fibres and weakest when shear forces are applied at their insertions in to bone. Ligaments are viscoelastic15 and display the viscoelastic properties of creep, stress relaxation and hysteresis. Beyond the ultimate stress there may be low resistance to elongation, resulting in a ligament that is intact but very lax. Ligaments do not function homogeneously; they are composed of functional bands, which come under tension at different joint positions. I Non-linear region: the tendon starts off relatively non-stiff and becomes progressively stiffer with increasing elongation. This region probably reflects straightening out of the crimping of the collagen fibres. Haemorrhagic/inflammatory phase Formation of haematoma Invasion by polymorphonuclear cells and monocytes/ macrophages with release of cytokines and growth factors Debris removed and replaced with fibroblasts and capillary buds. Muscle Structure Remodelling phase Collagen fibres reorganize to become orientated along the long axis of the tendon the basic muscle cell, or fibre, which is surrounded by the basal lamina. Within the muscle cells there is a hierarchical arrangement of contractile elements Fundamental units are actin and myosin molecules, which are arranged linearly. The myofibrils are mechanically connected to each other by proteins, mainly desmin; the muscle fibres are surrounded by epimysium the muscle fibres, or cells, are in turn are grouped in to fascicles surrounded by a perimysium Fascicles are grouped in to a muscle surrounded by an epimysium. Secondary afferent endings (flower spray fibres), sensitive to steady level tension. These three types are often equated to slow oxidative, fast oxidative and glycolytic, and fast glycolytic, respectively, although this is probably not justified. Fibre types are not immutable and fibres can change their type in response to their mechanical environment. Muscle contraction Muscle contraction is initiated by release of acetylcholine at the neuromuscular junction the acetylcholine diffuses in to the synaptic clefts Muscle contraction is controlled by calcium, which is stored in, and controlled by, the sarcoplasmic reticulum Calcium is transmitted in to the muscle via the transverse tubular system (T system) Calcium binds to troponin on the actin filaments, thus releasing the actin filament and enabling it to interact with the myosin, resulting in contraction Contraction velocity of muscle is proportional to fibre length. Types of muscle contraction Isotonic (dynamic) Muscle tension is constant through the range of motion Muscle length changes. Isometric (static) Muscle tension is generated but the length of the muscle remains unchanged. Muscle spindle Isokinetic (dynamic) Muscle tension is generated as the muscle contracts at a constant velocity over a full range of motion. Sensory structure within a muscle that regulates tension and acts as a proprioceptive organ: Primary afferent endings (annulospiral fibres), which respond mainly to the rate of change of length Concentric contraction Muscle shortens during the contraction. Eccentric contraction Muscle lengthens whilst contracting against an opposing force. The net result is that the junction is very strong this area has a specific morphology, which is adapted to its function. Specific features include: shorter sarcomere lengths, greater synthetic ability, greater number of organelles per cell, interdigitation of the cell membrane and intracellular connective tissue.
A perilunate dislocation demonstrates a capitate that is posterior or anterior to the lunate blood pressure chart stress discount coumadin 2mg, while the lunate maintains contact with the distal radius blood pressure chart diastolic cheap coumadin 1mg without prescription. The anteroposterior view is less specific and shows an obliterated joint space between the lunate and the capitate. Treatment involves anatomical alignment with closed reduction, though open reduction may be necessary. It is a transverse fracture of the distal radius metaphysis, which is dorsally displaced and angulated. The usual mechanism is a fall on an outstretched hand, and the wrist may demonstrate the classic "dinner fork" deformity on exam. The treatment is usually closed reduction, though more comminuted and displaced fractures will need open reduction and fixation. It results from a fall on a flexed wrist or a direct blow to the dorsum of the wrist. Photograph of the classic "dinner fork" deformity seen with dorsal radius fractures (left). Barton Fracture Barton fracture is a distal radius fracture in which the carpus displaces volarly with the radial fragment. A reverse Barton fracture is actually more common in which the carpus displaces dorsally with a fragment of the distal radius. Injuries may encompass two fractures at similar or separate sites or may involve a single fracture with ligamentous injury, with or without dislocation. Careful examination of the wrist and elbow joints is imperative, as these are commonly involved sites. Some common patterns are seen in forearm fractures and thus knowledge of these injury patterns is important. Both bones fractures (involving both the radius and ulnar shafts) are often seen in children secondary to falls on an outstretched hand. They are only rarely seen in adults and are then from high-energy mechanisms or severe direct impact. Closed reduction is often successful in children because small amounts of residual angulation will resolve with bone remodeling. Complete fractures are more common in adults, and open reduction is often required. The Monteggia fracture complex, first described in 1814, is a proximal ulnar fracture with an associated radial head dislocation. The injury is caused by forced pronation of the forearm during a fall on an outstretched hand. Radiographs easily reveal the proximal ulnar fracture, and in these cases the radial head should be carefully evaluated. In the normal position, the radial head should align with the capitellum when a line is drawn through the radial shaft. The injury occurs with a fall on an outstretched hand with wrist in extension and the forearm forcibly pronated, or with a direct blow to the dorsoradial aspect of the wrist. The anteroposterior radiograph reveals a fracture of the radius at the junction of the middle and distal thirds, and an increase in the joint space between the distal radius and ulna may be seen. In proximal ulnar fractures, the radial head should be carefully examined to exclude the presence of a Monteggia fracture. Associated injuries are rare but include compartment syndrome and vascular injury. Most undisplaced fractures are treated with plaster immobilization, while displaced fractures (>50% of width of ulna) may need open reduction. They are usually the result of a fall on an outstretched hand with arm extended and abducted.