Nizoral
"Buy nizoral 200 mg on line, fungus yellow".
By: L. Lee, M.B.A., M.D.
Program Director, Donald and Barbara School of Medicine at Hofstra/Northwell
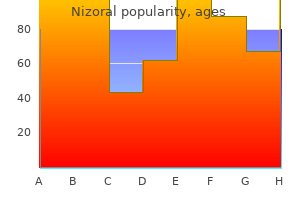
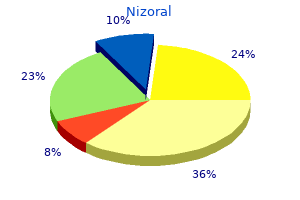
Eighty-eight percent reported minimal activity limitations and 84% rated school performance as average or above-average antifungal used to treat thrush buy nizoral with american express. Despite these encouraging parental perceptions fungus gnats basil buy generic nizoral canada, one-third of these children were receiving special education services. Longer waiting time prior to transplantation was found to have a negative effect on later neurocognitive outcomes. Surgical approach, staged palliation versus transplantation, was not associated with any measure of developmental outcome in a group of 47 school-aged children representing four institutions. Wernovsky and Newburger (403) postulated that these similar findings, despite dramatically different treatment strategies, are evidence of the important impact of genetic factors, congenital brain abnormalities and insults incurred during the pre- and perioperative period. In the Pediatric Heart Network cross-sectional study of 537 Fontan survivors at 6 to 18 years of age, parents reported problems with attention in 46%, learning in 43%, development in 24%, and behavior in 23% (398) demonstrating the wide spectrum of neurologic impact of complex heart disease. However, operative factors typically only account for a small portion of the variance in outcomes (241,393,394,404,405). However, the mean scores for each domain were within normal limits for all groups (406). Postoperative Sv02 values <40% were independently associated with poorer developmental outcomes. These studies have evaluated children at multiple different ages and stages of repair. Their findings will serve as a guide for future care and provide important information for counseling children, families, educators, and other health care practitioners. The definition of quality, however, can be provided only by the children and families living the experience. Parents reported that their children had more social problems and decreased activities, and were more withdrawn than healthy children. Teachers also reported children with single-ventricle heart disease to be more withdrawn in the classroom setting. Sixty-fivepercent of these children attended school full-time, and 27% attended half-time or more. School adjustment in the children was found to be significantly related to both family strain and exercise tolerance. The authors speculated that differences in parental expectations during early childhood may account for these different responses. The study identified scores for quality of physical health that were approximately one standard deviation below normal and scores for psychosocial health that were one-half standard deviation lower than normative values for the Child Health Questionnaire. In the majority of health status domains, parents reported worse physical and psychosocial function than children reported for themselves (425). Despite some physical limitations, the interviewer commented, "She seems to thrive within the context of her life. Although the early and intermediate outcomes in terms of survival have improved over the last decade, considerable challenges remain including options for the failing circulation, optimizing long-term neurodevelopmental outcome, and justifying allocation of increasingly scarce health care resources to a complex group of patients. Prevalence, treatment, and outcome of heart disease in live-born children: a prospective analysis of 91,823 live-born children. The determinants of five-year survival of infants with with critical congenital heart disease. Aortic atresia: Morphologic characteristics affecting survival and operative palliation. Familial risks of congenital heart defect assessed in a population-based epidemiologic study. Cardiac malformations in relatives of infants with hypoplastic left-heart syndrome. Acquired neuropathologic lesions associated with the hypoplastic left heart syndrome. Plasma amino acids in interrupted aortic arch and the hypoplastic left heart syndrome. Excess birth prevalence of hypoplastic left heart syndrome in eastern Wisconsin for birth cohorts 19971999. Seasonality of hypoplastic left heart syndrome in the united states: a 10-year time-series analysis.
Discrete subaortic stenosis: incidence fungus joint pain 200mg nizoral sale, morphology and surgical impact of associated subaorric anomalies fungus normal plague inc cheap nizoral 200mg amex. The genetics and pathology of discrete subaortic stenosis in the Newfoundland dog. Surgery for discrete subvalvular aortic stenosis: actuarial survival, hemodynamic results, and acquired aortic 1043 regurgitation. The syndrome of supravalvular aortic stenosis, peripheral pulmonary stenosis, mental retardation and similar facial appearance. Complete physical map of the common deletion region in Williams syndrome and identification and characterization of three novel genes. The aortic root in supravalvular aortic stenosis: the potential surgical relevance of morphologic findings. A developmental complex including supravalvar stenosis of the aorta and pulmonary trunk. A 20-year clinical perspective with patch aortoplasty, Am] Cardiel 1983;51: 256-260. Progressive left main coronary artery obstruction leading to myocardial infarction in a child with Williams syndrome. Generalized arterial fibromuscular dysplasia and myocardial infarction in familial supra valvular aortic stenosis syndrome. Pathology of coronary arteries, myocardium, and great arteries in supra valvular aortic stenosis. Myocardial infarction leading to sudden death in Williams syndrome: report of three cases. Forty-one years of surgical experience with congenital supra valvular aortic stenosis. An explanation of asymmetric upper extremity blood pressures in supra valvular aortic stenosis. Natural course of supravalvar aortic stenosis and peripheral pulmonary stenosis in Williams syndrome. Three decades of follow-up of aortic and pulmonary vascular lesions in the Williams-Beuren syndrome. Diagnosis and post-operative evaluation of supravalvular aortic stenosis by magnetic resonance imaging. The natural course of supravalvar aortic stenosis and peripheral pulmonary artery stenosis in Williams syndrome. Acute aortic insufficiency complicating stent treatment of supra valvular aortic stenosis: successful release of trapped leaflets by wiring the stent. Surgical management of left coronary artery ostial atresia and supravalvar aortic stenosis. Extended aortic and left main coronary angioplasty with a single pericardial patch in a patient with Williams syndrome. However, considerable variation exists in coarctation anatomy as well as in its pathophysiology, clinical presentation, treatment options, and outcomes. For example, although often a discrete stenosis, coarctation may be a long segment in nature, may be associated with hypoplasia of the transverse aortic arch (common in infancy), or may be abdominal in location. The pathophysiology of coarctation varies with the severity of the stenosis, and also is affected by the presence of associated lesions, such as patent ductus arteriosus, ventricular septal defect, or left ventricular outflow obstruction. The clinical presentation of coarctation also varies, ranging from heart failure in infancy to asymptomatic hypertension and/or a murmur in an older child or adult. Treatment options include surgery (most commonly resection and end-to-end anastomosis) and percutaneous balloon angioplasty and stenting. In many patients, the late prognosis is affected by residual coarctation stenosis or arch hypoplasia, associated intracardiac pathology, and resting or exercise hypertension. It is correct to conclude that coarctation of the aorta is not the simple lesion it often appears to be. The gross morphology of coarctation includes an intimal and medial malformation and a prominent posterior infolding (the posterior shelf), which, in some cases, extends around the entire circumference of the aorta (10). In infants, particularly those with associated left-ventricular outflow obstruction or a ventricular septal defect, there may be diffuse hypoplasia of the transverse aortic arch. Less commonly, coarctation of the aorta occurs in other locations, such as the ascending aorta or the abdominal aorta. Coarctation of the abdominal aorta is a complex long-segment stenosis that typically is associated with renal artery stenosis.
The level of systemic arterial oxygen saturation data reflects the magnitude of pulmonary blood flow fungi quote order nizoral uk. Before the era of routine administration of prostaglandin fungus roots buy nizoral amex, these infants became progressively hypoxemic coincident with functional and anatomic closure of the arterial duct. Unless there is pulmonary disease, the pulmonary venous saturation is normal, or nearly so. The administration of prostaglandin, by virtue of its action on the arterial duct and the pulmonary vascular resistance, augments pulmonary blood flow, and thus arterial saturation increases. The hemodynamic evaluation of the patient with the hypertensive right ventricle establishes right ventricular pressure at or above systemic levels. When dealing with the patient with massive cardiac enlargement, right ventricular pressure may be substantially less than systemic. The topography In the presence of nonrestrictive interatrial communication, the atrial mean pressures equalize, although there is often a small "a" wave gradient from the right to the left atrium. If true restriction to atrial flow is demonstrated then it is important to consider a balloon atrial septostomy at catheterization to avoid a low cardiac output syndrome, especially if decompression of the right ventricle is not to be included in the therapeutic track. The right ventricle is at systemic levels of pressure or higher, and the end-diastolic pressure may be abnormally high, consistent with a noncompliant ventricular chamber. The finding of a subsystemic right ventricular pressure is consistent with a globally disadvantaged right ventricle. The right ventricle is usually thinned, and severe tricuspid regurgitation often is present. The functional disturbance of severe tricuspid regurgitation correlates with an Ebstein-like abnormality of the tricuspid valve or severe tricuspid valve dysplasia. When right ventricular angiography does not demonstrate ventriculocoronary connections, one can be reasonably certain that coronary arterial stenosis or interruption or major fistulae with coronary-cameral flow will not be evident. In some patients with ventriculocoronary connections, a balloon catheter inflated in the right ventricle or catheter-induced tricuspid insufficiency with concurrent observation of the simultaneous electrocardiographic tracing may unmask a right ventricular-dependent coronary circulation. The angiocardiographic investigation of the patient with the hypertensive right ventricle requires right ventricular angiocardiography in frontal and lateral projections. The reported surgical survival of 27% prior to the availability of prostaglandins was poor (57). Rarely an urgent balloon atrial septostomy may be required for a restrictive septum as pulmonary flow improves and should be considered in any neonate that demonstrates persistent low cardiac output with the usual therapeutic maneuvers. For the premature infant or the extremely small-for-gestational-age infant, a prolonged course of an E-type prostaglandin may be necessary before surgery is undertaken, although this is unusual in the current surgical era. Once pulmonary blood flow is established, it is important to recognize that systemic oxygen saturation is related to the amount of flow into the pulmonary circulation. The patient has an obligatory rightto-left shunt at atrial level, hence a very high saturation usually reflects an enormous amount of pulmonary flow. The resulting low diastolic pressure and low cardiac output syndrome can result in compromised splanchnic and renal flow as well as ongoing acidosis and, in the extreme, cardiogenic shock. In addition, this physiology can compromise oxygen delivery to the aortocoronary circulation resulting in myocardial ischemia. The pulmonary outflow tract in this patient with valvar atresia is imaged in the precordial short-axis view with slight clockwise rotation. Lower Panel: the possibility of pulmonary insufficiency (red flow) raises the possibility that the valve is severely stenotic and not atretic. Selective injection of the right ventricular outflow tract can differentiate severe stenosis of the pulmonary valve from membranous atresia (56). Aortography in the neonate defines the laterality of the aortic arch, the caliber of the subclavian arteries, the site of insertion of the arterial duct, the caliber of the pulmonary arteries, and coarctation of the pulmonary artery at the insertion of the arterial duct that may preclude treatment with a stent to permanently maintain its patency or require a surgical patch at the time of placing a Surgical Surgical and other catheter-based interventional therapies have continued to change with an understanding of the heterogeneity of this disorder. The diagnostic and therapeutic algorithms are now quite diverse, depending on a wide number of morphologic variables (5,58-62). Among some centers, primary cardiac transplantation also is considered particularly when the coronary artery anatomy is complex. Functional pulmonary atresia in a newborn with pulmonary atresia and intact ventricular septum.
Primary graft failure and early morbidity are largely explained by recipient issues that increase perioperative risk (110) fungus weed discount nizoral 200mg otc. Acute renal failure occurs postoperatively in 3% to 10% of transplant recipients (111) antifungal shampoo for horses order nizoral with american express. Multidisciplinary team management including nephrology consultation is often useful in this circumstance. Patients often develop systemic hypertension in the immediate postoperative period. This can be secondary to baroreflex-mediated hypertension, catecholamine dysregulation from low cardiac output before transplant, significant preexisting renal injury, and newly initiated immunosuppressive medications such as corticosteroids or calcineurin inhibitors. Treatment consists of antihypertensive medication titration to achieve a normal blood pressure for age. An inappropriately small donor heart size has been associated with increased mortality, and a donor/recipient weight ratio <1 has been reported as a significant predictor of fatal postoperative heart failure (112). Postoperative pericardial effusions develop in 9% to 21 % of adult recipients (113,114). The incidence in pediatric patients is unknown but is likely similar to adults and may, in part, be related to an increased pericardial volume created after a dilated heart is replaced with normal-sized heart that fills with fluid. Unless the effusion is hemodynamically compromising or there is a strong suspicion of an infectious etiology, the effusion usually does not require surgical or percutaneous drainage and can be monitored serially by echocardiography. Posttransplant sinus node dysfunction is common with a reported prevalence as high as 44% (115) and is likely related to myocardial ischemia and surgical manipulation. High-dose corticosteroids are given intraoperatively and continued for a brief period of time, after which they can be discontinued or decreased to a low-dose maintenance regimen. Over the last 12 years, the incidence of rejection in the 1st year after pediatric heart transplant has decreased from about 60% to just over 40% (119). The peak hazard, or instantaneous risk, for rejection is around 1 to 2 months after transplantation (120). Older age at transplantation represents a risk for first rejection and a risk for an increased number of episodes of rejection within the first 6 months after transplantation. Infections occur in up to 25% of pediatric recipients during the early postoperative period, and 60% of these infections are bacterial (121). Bloodstream and pulmonary infections are most common, followed by urinary tract and surgical site infections (123,124). Because of the inconvenience, greater technical challenges, and possible increased morbidity of biopsy in smaller children, there has been much interest in evaluating the role of echocardiography in children undergoing transplantation (125-131). Despite this interest, the controversy over the role of echocardiography is far from resolved. In fact, many centers have discontinued routine surveillance biopsies after the 1st or 2nd year from transplantation. Many centers perform routine endomyocardial biopsy on infants significantly less frequently or not at all, instead depending on physical exam and echocardiogram to aid in diagnosis, and reserve biopsy only for clinical indications (136). With any clinical deterioration in the early postoperative period, evaluation of and treatment for rejection as the potential cause should be considered. The need for noninvasive diagnosis of rejection has stimulated the ongoing search for biohumoral markers, such as B-type natriuretic peptide. Clinical evaluation of rejection is important but can be misleading, particularly in pediatric patients in whom infectious issues can mimic the presentation of rejection. The characteristic infiltration of the donor heart by lymphocytes leads to the diagnosis of rejection on endomyocardial biopsy (141). The surface electrocardiogram may suggest atrial flutter or atrioventricular dissociation, but this observation may be attributed to the fact that the recipient atrial tissue contracts independently of the donor atrial tissue, and there may be two P waves present on the surface electrocardiogram that are not synchronous. The vast majority of initial rejection episodes can be successfully reversed by high-dose corticosteroids alone or in conjunction with anti- T-cell antibodies. Corticosteroids as either intravenous methylprednisolone (10 to 30 mg/kgevery 12 hours) or oral prednisone are the first line in rejection therapy. Pathologically, this form is characterized by a lack of significant cellular rejection on endomyocardial biopsy with characteristic histologic and/or immunohistochemical findings (145,146). It is often accompanied by left ventricular dysfunction and detection of donor-specific antibodies in the recipient serum.
Medical management includes optimizing caloric intake and weight gain fungus on plants buy nizoral with american express, monitoring for the possible development of pulmonary hypertension and atrial arrhythmias fungus packaging buy nizoral with paypal, aggressive management of respiratory infections, influenza vaccinations, and prophylaxis against respiratory syncytial virus infection with palivizumab for children <2 years of age. Freedom from reintervention was 80% at 10 years, and survival was approximately 95% at 15 years and approximately 85% at 20 years. These excellent results demonstrate the feasibility of a conservative surgical approach. The relationship of mitral annular shape to the diagnosis of mitral valve prolapse. A study of functional anatomy of aortic-mitral valve coupling using 3D matrix trans esophageal echocardiography. Geometric changes of mitral annulus assessed by real-time 3-dimensional echocardiography: becoming enlarged and less nonplanar in the anteroposterior direction during systole in proportion to global left ventricular systolic function. Restricted diastolic opening of the mitral leaflets in patients with left ventricular dysfunction: evidence for increased valve tethering. Two-dimensional versus transthoracic real-time three-dimensional echocardiography in the evaluation of the mechanisms and sites of atrioventricular valve regurgitation in a congenital heart disease population. Left ventricular function after resection of the papillary muscles in patients with total mitral valve replacement. Anatomic types of congenital mitral stenosis: report of 49 autopsy cases with consideration of diagnosis and surgical implications. The developmental complex of "parachute mitral valve," supravalvular ring of left atrium, subaortic steno- in the Pediatric Population 1021 27. Anomalous mitral "cleft" with abnormal ventriculo-arterial connection: anatomical findings and surgical implications. Comparison of cleft and papillary muscle position in cleft mitral valve and atrioventricular septal defect. Abnormalities of the mirral valve in congenitally correcred transposition (discordant atrioventricular and ventriculoarterial connections). Direct measurement of vena contracta area by real-time 3-dimensional echocardiogrpahy for assessing severity of mitral regurgitation. Real-time three-dimensional echocardiography provides new insight into the mechanisms of tricuspid valve regurgitation in patients with hypoplastic left heart syndrome. Factors influencing pulmonary venous flow velocity patterns in mitral regurgitation: an in vitro study. Usefulness of live/real time threedimensional transthoracic echocardiography in the identification of individual segment/scallop prolapse of the mitral valve. Head-to-head comparison of two- and three-dimensional transthoracic and transesophageal echocardiography in the localization of mitral valve prolapse. Cardiovascular magnetic resonance for direct assessment of anatomic regurgitant orifice in mitral regurgitation. Palivizumab prophylaxis reduces hospitalization due to respiratory syncytialvirus in young children with hemodynamically significantcongenital heart disease. Aortic and mitral valve replacement in children: is there any role for biologic and bioprosthetic substitutes Echocardiographic predictors of mitral stenosis-related death or intervention in infants. Isolated congenital mitral valve regurgitation presenting in the first year of life. Late left ventricular function after surgery for children with chronic symptomatic mitral regurgitation. Mitral valve replacement with mechanical prostheses in children: improved operative risk and survival. Long-term survival after mitral valve replacement in children aged <5 years: a multi-institutional study. Congenital aortic stenosis occurs in different forms, usually classified with respect to the location of the obstruction relative to the aortic valve: valvular, subvalvular, or supra valvular. Because the clinical features and treatment of these forms of aortic stenosis differ, they are discussed separately in this chapter. Although this chapter deals primarily with congenital aortic stenosis and not hypoplastic left heart syndrome, the infant with severe aortic stenosis and small left ventricle presents important therapeutic issues that justify separate discussion (see Chapter 48). Autopsy studies have reported that congenital bicuspid aortic valve occurs in approximately 1.