Rocaltrol
"Best 0.25mcg rocaltrol, symptoms weight loss".
By: D. Tarok, M.B. B.CH. B.A.O., M.B.B.Ch., Ph.D.
Vice Chair, Rutgers Robert Wood Johnson Medical School
It is most helpful in cases of penetrating trauma (especially gun shot or knife wounds) to assess for nerve continuity medicine for sore throat cheap 0.25 mcg rocaltrol fast delivery. The other rare situation in which ultrasound is helpful is in assessing the sciatic nerve for tumors affecting the nerve directly medicine merit badge rocaltrol 0.25 mcg cheap. Top left, Long axis view of the sciatic nerve in the distal thigh, demonstrating a hyperechoic bony shadow (red arrow) near a normal appearing sciatic nerve. The right side of the photo is proximal, with surgical bands around the sciatic, tibial, and peroneal nerves. Note the surgical clamp grasping a large piece of bone (green arrow), which was impinging on the sciatic nerve. In this case, ultrasound was essential in not only allowing the identification of the traumatic bone spicule but also demonstrating its relationship to the sciatic nerve. Jonathan Miller, Department of Neurological Surgery, University Hospitals Cleveland Medical Center. In these cases, the tumor is located within the nerve proper and often associated with increased vascularity on ultrasound. An example of a structural lesion affecting the sciatic nerve, diagnosed by neuromuscular ultrasound, follows here. She initially noted a sensation of numbness over the top of the foot and the lateral calf. During the last 2 months, symptoms slowly progressed to a nearly complete foot drop. More recently, she noted a sensation of tightness and pain from her hip down to her knee and into her calf. Example: Sciatic Neuropathy Secondary to a Bone Fragment A 14-year-old girl sustained a comminuted fracture of the distal femur and underwent surgical fixation. Past history was notable for a left hip fracture with surgical repair 3 years previously. Deep tendon reflexes were 2+ and symmetric in the upper extremities and 2+ at the knees and right ankle. There was a clear sensory disturbance to light touch on the top of the foot, lateral foot and calf, lateral knee, and posterior calf on the left side. Sensation over the medial calf, anterior thigh, lateral thigh, posterior thigh, and sole of the foot was intact. Summary the initial clinical presentation is that of a foot drop with numbness over the dorsum of the foot and lateral calf. Most often, this clinical picture is the result of a peroneal neuropathy at the fibular neck. However, an early sciatic neuropathy, lumbosacral plexopathy, or lumbosacral radiculopathy (especially L5) can present in a similar fashion. The slowly progressive nature of the symptoms suggests a slowly expanding or infiltrating structural lesion. As the symptoms progressed, the patient noted a sensation of tightness and pain from the hip toward the knee into the calf. These additional symptoms would be unusual for a peroneal palsy at the fibular neck and are suggestive of a more proximal lesion. Neurologic examination showed severe weakness and atrophy in the distribution of the deep and superficial peroneal nerves (ankle and toe dorsiflexion, ankle eversion). In addition, there was weakness of knee flexion, which is subserved by the sciatic nerve. Further testing of muscles innervated by the femoral, superior gluteal, inferior gluteal, and obturator nerves was normal. The absence of abnormalities in these muscles on clinical examination suggests that a more widespread lesion of the lumbosacral plexus or nerve roots was unlikely. Of course, early in any lesion, it may be difficult to demonstrate subtle weakness of the proximal limb muscles. Moving on with the clinical examination, the left ankle reflex was absent, signifying a lesion somewhere along that reflex loop, in the tibial nerve, sciatic nerve, lumbosacral plexus, or lumbosacral nerve roots. Normal sensation was found in the medial calf, innervated by the saphenous nerve; the anterior thigh, innervated by the femoral nerve; the lateral thigh, innervated by the lateral cutaneous nerve of the thigh; and the posterior thigh, innervated by the posterior cutaneous nerve of the thigh. This distribution of sensory abnormalities again suggests a lesion at or proximal to the sciatic nerve.
In most cases medicine 657 buy 0.25mcg rocaltrol with amex, if there is any evidence of axonal continuity medicine you cannot take with grapefruit rocaltrol 0.25mcg overnight delivery, further observation is indicated before surgical intervention. The vast majority of these lesions are axonal rather than demyelinating, so motor conduction studies across the brachial plexus (although theoretically appealing) most often are not helpful. In addition, radial and median sensory responses may be abnormal, especially when recording the thumb. Most important, the rhomboids, serratus anterior, and cervical paraspinal muscles are spared, unless the lesion also involves the nerve roots. When closely observed, one will note that the firing only occurs when the patient breathes, specifically during inspiration. Any trauma that injures the C5 root before the branch to the phrenic nerve can result in this syndrome. In addition, abnormalities may be seen in the deltoid, teres minor, and latissimus dorsi. Because the median- and ulnar-innervated hand muscles are derived from the medial cord, their respective motor studies and F responses may be abnormal as well. Whereas both ulnar and medial antebrachial cutaneous sensory fibers travel through the lower trunk, median sensory fibers are derived from the upper and middle trunks. Although both median- and ulnar-innervated motor fibers travel through the lower trunk, the median-innervated thenar muscles typically are more affected than are the ulnar-innervated hypothenar muscles, probably reflecting greater T1 innervation of thenar compared with hypothenar muscles. Median and ulnar distal latencies and conduction velocities may be slightly slowed. The ulnar sensory response, however, is abnormal because the ulnar sensory fibers travel through the lower trunk. The ulnar sensory response is abnormal because the ulnar sensory fibers travel through the lower trunk. However, this report utilized nerve root stimulation and collision studies to demonstrate the blocks, both of which are difficult to perform. When abnormal, they are frequently borderline low and need to be compared with the contralateral side. Of the sensory studies available, the lateral antebrachial cutaneous has the highest yield of being abnormal followed by the medial antebrachial cutaneous. Thus, even though a nerve may be involved that has cutaneous sensory fibers, if only the distal branch to a muscle is affected, the sensory fibers in the parent nerve will not be affected. However, as one samples more muscles, there are frequently changes in other muscles which appeared clinically unaffected. Similarly, if one samples the contralateral unaffected side, it is not infrequent that mild changes are present as well, again implicating a more widespread and patchy disorder. As all muscles are supplied by two if not three myotomes, marked weakness is distinctly unusual in a radiculopathy. A combination of continuous adjustments of pressure, alignment, and rotating and tilting the probe is needed to identify landmarks and recognize structures. As such, neuromuscular ultrasound of the brachial plexus should be learned and performed only after one has obtained mastery in ultrasound of the common mononeuropathies. Ultrasound of the brachial plexus has significant challenges but also significant advantages. In addition, ultrasound does not have the ability to visualize structures behind bone. Since much of the brachial plexus is located beneath and below the clavicle, these areas are either inaccessible or difficult to access with ultrasound. Nevertheless, ultrasound of the brachial plexus offers some unique advantages in the recognition of certain disorders. The root level requires needle stimulation that is painful and difficult for patients, in addition to the obvious technical difficulties of obtaining supramaximal stimulation and ensuring correct needle localization. However, obtaining supramaximal stimulation and preventing co-stimulation of adjacent nerves are frequent problems.
Asthe primary medical conditions are treated and begin to recover treatment 3rd degree hemorrhoids buy rocaltrol with a visa, the sedatives and other drugs are weaned in preparation for extubation medications quizlet discount rocaltrol 0.25mcg mastercard. However, despite apparently intact cardiac and pulmonary function, the patient fails to wean off the ventilator. The question then arises if there is a neuromuscular disorder that is preventing extubation. Acute motor neuron disease is very uncommon and occurs only in the setting of paralytic poliomyelitis. Other variants have been described, including axonal forms, one of which is motor andsensory,andtheotherpuremotor. In addition to severe polyneuropathies, mononeuropathies of one or both phrenic nerves can directly result in respiratory compromise. In addition, phrenic neuropathy can occur rarely as part of neuralgic amyotrophy, either in isolation or more commonly as part of a more widespread pattern of multiple mononeuropathies. The other situation where unilateral or bilateral phrenic neuropathies occurs is as a complication ofthoracicsurgery. The typical presentation is one of descending paralysis, often associated with gastrointestinal and autonomic symptoms. Second, the disorder usually presents subacutely over months, and respiratory muscles are not typically involved. These patients typically are intubated and treated with high-dose intravenous methylprednisolone. As the asthma improves, it becomes apparent thatthepatientisflaccid,areflexic,andprofoundlyweak. Finally, although extremely rare, the myopathy associated with adult-onset acid maltase deficiency characteristically affects respiratory and abdominal muscles and can present as a primary neuromuscular cause of respiratory insufficiency. Some agents, such as propofol, can be easily adjusted Use 50-Hz repetitive nerve stimulation Choose muscles that will contract reflexively when withdrawing from a painful stimulus One person holds the leg with the knee flexed, taking care not to touch recording electrodes, while the second person stimulates Study the tensor fascia lata or gluteus medius; they are in the lateral thigh when supine Study the medial or anterior deltoid Omit; if absolutely necessary, need additional personnel to help roll the patient Omit the H reflex; if absolutely necessary, can be performed supine Do not do any electrodiagnostic studies-risk of electrical injury too high Study contralateral side; if not possible, avoid proximal stimulation. On the other hand, patients who are intubated are often sedated with benzodiazepines or narcotics. Neithertheagitated patient nor the sedated patient is able to give the electromyographer proper feedback during the study, for example whether he or she is feeling the stimulus during thenerveconductionstudies. Norcansuchpatientsplace their limbs in the correct position for the nerve conduction studies or the spontaneous activity assessment portion oftheneedleexamination. The presence of arterial lines, especially at the wrist, often interferes with the ability to stimulate the distalmedianandulnarnerves. Becausetheantecubitalfossa is a common site for intravenous lines, the proximal median stimulation site may not be accessible. This can be remedied by moving more proximally toward the axilla where the median nerve can often be easily stimulated. AsnotedinChapter22, if ulnar motor conduction studies are not performed with the elbow in a flexed position, factitious slowing across the elbow may easily occur. If the patient cannot be rolled onto the contralateral side or maintain that position, the study can be done with the patient supine and thelegflexedattheknee. Most important among them are the gluteal, hamstring, posterior shoulder girdle, and paraspinal muscles. These beds usually are electrical devices themselves, with motors, wires, and controls as part of the actual bed. Thus nerve conduction studies often are normal initially, except for the Fresponses,whicharedelayed,impersistent,dispersed,or absent. In the case of absent F responses, however, there is one very important proviso before attributing absent F responses to proximal demyelination. Recall that the circuitry of the F response includes the anterior horn cell in the spinal cord. Likewise, the anterior horn cell is susceptible to suprasegmental inhibitory influences. Thus, if a patient is heavily sedated or in coma, absent F responses are of no significance and may be a normal finding in this population. Thispattern is distinctly unusual in most myopathies, which preferentially affect proximal muscles, which are not recorded in routine nerve conduction studies. Even in the unusual case of adult-onset acid maltase deficiency, distal muscles are not affected. Each pattern suggests a specific localization; in some cases, the pattern may suggest additional studies to be performed.
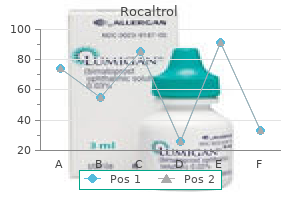
Since the cathode position is unchanged symptoms 10 dpo discount rocaltrol 0.25mcg, the depolarization still occurs at the same location top medicine buy generic rocaltrol canada. However, the geometric relationship between the axis of the cathode-anode and the recording electrodes can dramatically affect the direction and influence of the volume conducted stimulus artifact potential. Finally, ensuring that the stimulator and recording electrode cables do not overlap and are kept as far apart as possible will help reduce the influence of the stimulus artifact. As will be discussed in Chapter 42 "Basics of Electricity and Electronics for Electrodiagnostic Studies," overlapping cables can much more easily allow a stimulus artifact to occur in the recording electrode cables from the electrical property of induction. Keeping the stimulator cable away from the recording electrode cables is one of the simplest and most effective ways of reducing stimulus artifact. One effective method to reduce stimulus artifact and obtain a clear baseline is to slightly rotate the anode of the stimulator one way or another while maintaining the position of the cathode (known as walking the anode). In this example, the superficial peroneal sensory nerve is stimulated in the lateral leg and recorded over the ankle. Note how the waveform changes as the anode is rotated between position 1 and position 2 while the cathode position is kept constant. In position 2, the waveform has a much improved baseline, which increases the accuracy of the onset latency and amplitude measurements. These potentials can be influenced by the geometry of the source in relation to the recording electrode. Cathode Position: Reversing Stimulator Polarity When a nerve is stimulated, depolarization first occurs beneath the cathode. For nerve conduction studies, the proper position of the stimulating cathode is facing the active recording electrode (remember: black to black). If the cathode and anode of the stimulator are inadvertently reversed, two effects are possible. This hyperpolarization may create a block, preventing the depolarization that occurs under the cathode from proceeding past the anode to the recording electrode. The issue of anodal block is more of a theoretic concern and is rarely seen in practice. Second, distal motor latencies will be similarly prolonged, but motor conduction velocities, which are calculated between a distal and a proximal site, will remain unchanged. With nerve stimulation, depolarization first occurs beneath the cathode and travels in both directions. The cathode should always face the active recording electrode (G1) (remember: black to black). To calculate a conduction velocity, distance is measured between the cathode and the active recording electrode. With stimulation, the nerve depolarizes beneath the cathode and travels in both directions, and the segment under the anode may hyperpolarize. This hyperpolarization may block the action potential that originates at the cathode and prevent it from proceeding past the anode. Median motor study, stimulating the wrist, recording the abductor pollicis brevis with increasing stimulator currents. To ensure that all axons are stimulated, supramaximal stimulation is required for all nerve conduction studies. Supramaximal stimulation is achieved by increasing the stimulator current until the recorded potential has reached maximal amplitude. To ensure supramaximal stimulation, the current should then be increased by an additional 25% to ensure that the amplitude does not increase further (bottom trace). Top trace reflects the correct position with the cathode facing the active recording electrode. Bottom trace reflects the cathode and anode reversed with the cathode facing away from the active recording electrode. Bottom, If the cathode and anode are inadvertently reversed, artifactual slowing of latency and conduction velocity occurs.

