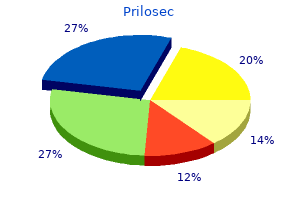
Prilosec
"Buy genuine prilosec on-line, chronic gastritis radiology".
By: V. Masil, M.A., M.D.
Medical Instructor, Florida International University Herbert Wertheim College of Medicine
Researchers have identified antibodies and fragments of prion protein (short synthetic protein molecules) that can block the conversion of normal prion protein to the abnormal form gastritis diet кинопоиск purchase 20mg prilosec amex. If successful gastritis diet 4 rewards order prilosec 40 mg online, these studies may lead to effective methods to prevent prion infections and to the development of therapies that work either in affected patients or in the presymptomatic phases of disease. Because the main site of treatment for prion diseases is in the brain, where much of the neuronal damage is caused, drugs administered intravenously need to cross the blood-brain barrier to be effective. It has helped persons who have thrombotic (blood clotting) disorders and interstitial cystitis (inflammation of the urinary bladder). However, the laboratory experiments did not show any affect when used as treatment for humans with prion diseases. Because little is known about how neurons die in persons with prion diseases, it is difficult to understand the mechanism by which this drug may work. One patient had suggestions of improved neurological condition, but judgment is difficult to ascertain, and another patient showed no successful response to the drug. Other scientific papers using this treatment on a few patients have been published, with inconclusive results; however, the research has led to further investigation, though caution is emphasized because of possible side effects and the risk of administering the drug. Much remains to be learned and understood about the use of flupirtine and other drugs for prion diseases after infection has occurred. To help with symptoms, persons with dysphagia or swallowing difficulties, for example, may need the feeding tubes. Impact One major dilemma in attempts to treat prion diseases is that persons with the disease are identified long after the disease has advanced. Therefore, treatments are less likely to help with symptoms or to improve the disease state. One approach for future treatment is to intercept the disease well before it deteriorates the brain and to diagnose the disease earlier in the disease state. Discusses the use of the drug quinacrine for clinical use in human prion diseases. Salem Health the pharmacological treatment of malaria can include chemoprophylaxis, or antimalarial medications, taken before a person travels to a geographic area at high risk for malaria; drugs administered during an acute attack; and drug therapy taken to prevent a relapse of illness. Chemoprophylaxis drugs are taken one week before travel to an infested (or endemic) area, during the stay there, and for one to four weeks after return from travel. If the infected person cannot take this drug, combinations of drugs such as atovaquoneproguanil (Malarone); mefloquine (Lariam), which is used by pregnant women; doxycycline; and primaquine may be prescribed. The earlier the treatment occurs in the course of the infection, the more likely therapy is to be successful. Because malarial symptoms can mimic a common cold, infected persons often delay seeing a health care provider for treatment or are often misdiagnosed. The first choice of pharmacological treatment for acute malaria is chloroquine, which interrupts the erythocytic stage of the infection and breaks the life cycle of the protozoan. If there is resistance to this drug, alternates are primaquine, mefloquine, quine sulfate, and atovaquone-proguanil. Antibiotics such as doxycyclin, clindamycin, and tetracycline (except in pregnant women) may also be administered. If infected persons have illnesses that are more progressed, they can be administered quinidine gluconate intravenously in combination with the foregoing antibiotics. Chloroquine, the primary medication used to treat malaria, is contraindicated in persons with retinal problems because it can cause irreversible damage to the retina when given in high doses. Because the drug is metabolized in the liver, persons with compromised liver function, such as in alcoholism, should use this drug with caution. People with a history of hematologic disease should consider an alternate drug choice, because chloroquine can cause blood dyscrasias. As with all medications, drug interactions should be considered before therapy begins. Amebiasis, a protozoan disease caused by the ingestion of Entamoeba histolytica, usually occurs in the human digestive system. However, amebiasis can spread through colon ulcers to other parts of the Treatment of protozoan diseases Category: Treatment Definition Treatment for protozoan diseases involves therapy to manage infections caused by living, single-cell, parasitic, and eukaryotic organisms known as protozoa. Common Protozoan Diseases Common protozoan diseases are malaria, amebiasis, toxoplasmosis, and trichomoniasis, which, along with their treatment protocols, are discussed here.
Alternatively gastritis rectal bleeding purchase 10mg prilosec overnight delivery, elevating the head to a 25-degree back-up position (keeping the patient supine while placing the bed in 25-degree reverse Trendelenburg) may achieve the same purpose gastritis symptoms fatigue cheap 20mg prilosec otc. If this is noted, the head can be raised until the head and neck are in neutral position. To maintain the best mechanical advantage, keep your back straight and do not hunch over the patient. Keep the left elbow relatively close to the body and flex it slightly to provide better support. If you initially place the blade in the middle of the tongue, it will fold over the lateral edge of the blade and obscure visualization of the airway. The direction of this force is critical because if the force is too horizontal or too vertical, poor visualization will result. Avoid bending the wrist because it can result in dental injury if the teeth are used as a fulcrum for the blade. It may help to have an assistant retract the cheek laterally to further expose the laryngeal structures. Locating the epiglottis is a crucial step in laryngoscopy, and has been termed epiglottoscopy. The step after visualization of the epiglottis depends on which laryngoscope blade is being used. Continued anterior elevation of the base of the tongue will partially lift the epiglottis. With the blade in the midline of the vallecula, engage the hyoepiglottic ligament with the tip of the blade to indirectly lift the epiglottis and expose the laryngeal inlet. If the tip of the blade is inserted too deeply into the vallecula, the epiglottis may be pushed down and obscure the glottis. If the straight blade is placed too deeply, the entire larynx may be elevated anteriorly and out of the field of vision. If the blade is deep and posterior, the lack of recognizable structures indicates esophageal passage; gradually withdraw the blade to permit the laryngeal inlet to come into view. The large head of newborns can result in a posterior positioning of the larynx that prevents visualization of the vocal cords. This is not necessary in all children; rather, the goal of any positioning maneuvers should be alignment of the tragus with the anterior shoulder. Do not allow the tube to obstruct your view of the vocal cords during advancement. A, the laryngoscope blade is under the middle of the tongue, with the sides of the tongue hanging down and obscuring the glottis. There is significant evidence that it can interfere with ventilation and intubation, so it is best to apply cricoid pressure on a case-by-case basis with a full understanding of the benefits and drawbacks of cricoid pressure. Note that in small children, the neck is shorter and the larynx is located more cephalad. If no laryngeal structures are visible after laryngeal pressure, gradually withdraw the blade. Do not place a towel under the occiput; a child may benefit from elevation of the shoulders. The large head may be "floppy" and require the assistant to hold the head still during intubation. Nasotracheal intubation in a child may cause excessive bleeding and is not recommended. Adenoid or tonsil tissue may plug the endotracheal tube or cause airway obstruction from aspiration. A more superiorly located larynx or an "anterior" larynx is more difficult to visualize. The epiglottis is more difficult to manipulate in a child; it may fold down and obstruct the view with use of a curved blade. For partial airway obstruction or to break laryngospasm, consider positive pressure ventilation with a jaw-lift maneuver to open the arytenoids. The anterior superior slant of the vocal cords may cause the endotracheal tube to hang up on the anterior commissure as it passes into the larynx.
Sedation should be targeted to a specific sedation scale (such as the Richmond Agitation Sedation Scale) gastritis diet шинэ buy 40 mg prilosec amex. Agents with a quick offset are preferable to improve spontaneous awakening and for breathing trials once the patient is a candidate for extubation gastritis diet 23 order prilosec online from canada. If paralyzing drugs are used for neuromuscular blockade, it is imperative to provide aggressive sedation because pain and anxiety in paralyzed patients cannot be evaluated. It is prudent to conclude that a paralyzed ventilated patient is awake and can hear and feel unless sedated. It is necessary to adequately sedate these patients because their hypercapnic state is a powerful stimulus to breathe rapidly. Opiates such as fentanyl and sedatives such as propofol and ketamine have gained increased roles in these patients. This should be a final option and be done with the understanding that the side effects of steroids and paralytics can be quite devastating,42,43 but paralysis cannot be avoided in certain cases. A common goal of blockade is to use enough of the agent to result in two twitches out of a "train of four. Valuable information can be gained from flow-time curves and pressure-time curves. The patient has to generate a decrease of only 7 cm H2O (instead of 12 cm H2O), thereby reducing the inspiratory effort required. If cardiovascular collapse occurs in a ventilated asthmatic with either pulseless electrical activity or sudden hypotension, a first step in troubleshooting is to remove the patient from the ventilator. A hyperinflated asthmatic lung severely diminishes venous return, which leads to a marked decrease in cardiac output, even pulseless electrical activity. If a recently intubated asthmatic suffers these consequences, stop ventilating the patient entirely (arrow), compress the chest until no more air is exhaled, and then continue ventilating as per discussion in text. Forty-one percent of patients never received recommended settings during hospitalization. Sedation needs to be optimized, and at times different modes, such as pressure-targeted modes, may be attempted. In dire circumstances, these modalities may be used on the basis of clinician preference and expertise and consultation with a critical care specialist. Tension pneumothoraces may be recognized by tachycardia, hypotension, elevated peak airway pressure (if mechanically ventilated, tachypnea if not), jugular venous distention, thoracic resonance by percussion on the affected side, diminished or absent breath sounds on the affected side, and tracheal deviation away from the affected side. Each of these catheters should be placed into a chest drainage collection unit that incorporates a water seal chamber and variable suction control. Treat persistent air leaks initially with continuous suction (usually suction at 20 cm H2O) to evacuate the pleural space and promote coaptation of the visceral and parietal pleurae. Reduce suction and place the chest tube on water seal only after resolution of any air leak. Remove the chest tube directly from the water seal if no pneumothorax is apparent on a chest film or after a test period of tube clamping and subsequent radiographic evaluation. The author favors a 4-hour period of clamping because recurrent pneumothorax is easier to treat by unclamping a tube than by placing a new one. Not all patients with a pneumothorax require invasive techniques to evacuate air from the pleural space. It is important to recognize that small pneumothoraces occurring in spontaneously breathing patients. Originally, this problem was thought to be caused by too much pressure (barotrauma). The end result is overdistention of the compliant segments, alveolar injury, liberation of inflammatory cytokines and chemokines, activation of endothelin and arachidonic acid pathways, and the expression of adhesion molecules along the vascular endothelium. Any process that impedes venous return will decrease the available volume that establishes cardiac output. If the ventilator settings lead to increased intrathoracic pressure during exhalation, venous return will be reduced. Venous return not only depends on a relatively negative pressure within the thoracic cavity but also relies on a sufficient amount of time for flow into the thoracic vasculature and right side of the heart. An additional untoward side effect of impaired venous return is cerebral venous hypertension from impeded venous drainage.
Combes X gastritis radiology order prilosec 40 mg with mastercard, Sauvat S gastritis que debo comer order 40 mg prilosec with mastercard, Leroux B: Intubating laryngeal mask airway in morbidly obese and lean patients: a comparative study. Asai T, Neil J, Stacey M: Ease of placement of the laryngeal mask during manual in-line neck stabilization. Ali A, Canturk S, Turkmen A, et al: Comparison of the laryngeal mask airway Supreme and laryngeal mask airway Classic in adults. Eschertzhuber S, Brimacombe J, Hohlrieder M, et al: the laryngeal mask airway Supreme-a single use laryngeal mask airway with an oesophageal vent. A randomised, cross-over study with the laryngeal mask airway ProSeal in paralysed, anaesthetised patients. Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Part 6: advanced cardiovascular life support: section 3: adjuncts for oxygenation, ventilation and airway control. The American Heart Association in collaboration with the International Liaison Committee on Resuscitation. Asai T, Matsumoto S, Shingu K, et al: Use of the laryngeal tube after failed insertion of a laryngeal mask airway. Agro F, Galli B, Ravussin P: Preliminary results using the laryngeal tube for supraglottic ventilation. Baraka A: Laryngeal mask airway for resuscitation of a newborn with Pierre-Robin syndrome. Brimacombe J, Gandini D: Airway rescue and drug delivery in an 800-g neonate with the laryngeal mask airway. Osses H, Poblete M, Asenjo F: Laryngeal mask for difficult intubation in children. Trawoger R, Mann C, Mortl M, et al: Use of laryngeal masks in the resuscitation of a neonate with difficult airway. Lopez-Gil M, Brimacombe J, Alvarez M: Safety and efficacy of the laryngeal mask airway. Brimacombe J, Keller C: Cervical spine instability and the intubating laryngeal mask-a caution. Kihara S, Watanabe S, Brimacombe J, et al: Segmental cervical spine movement with the intubating laryngeal mask during manual in-line stabilization in patients with cervical pathology undergoing cervical spine surgery. Waltl B, Melischek M, Schuschnig C, et al: Tracheal intubation and cervical spine excursion: direct laryngoscopy vs. Richez B, Saltel L, Banchereau F, et al: A new single use supraglottic airway device with a noninflatable cuff and an esophageal vent: an observational study of the i-gel. Uppal V, Fletcher G, Kinsella J: Comparison of the i-gel with the cuffed tracheal tube during pressure-controlled ventilation. Frass M, Frenzer R, Rauscha F, et al: Ventilation with the esophageal tracheal combitube in cardiopulmonary resuscitation. In Brimacombe J, editor: Laryngeal mask anesthesia, Philadelphia, 2005, Saunders, p 577. Paventi S, Liturri S, Colio B, et al: Airway management with the Combitube during anaesthesia and in an emergency. The primary objective of airway management is to maintain adequate ventilation and oxygenation, and intubation only allows ventilation and oxygenation after the procedure is completed, not during the procedure. It is also important to use intubation techniques that have a high likelihood of first pass success, to have the wisdom to recognize when a given approach has failed, and to quickly move to a different technique. Use of an emergency airway algorithm can help providers make difficult decisions in a timely manner (see later section on Emergency Airway Algorithm). Although flexible endoscopic devices are commonly used, with good topical anesthesia, nearly any intubating technique can be used for awake intubation.