Female Viagra
"Order female viagra amex, menstruation 1".
By: V. Frithjof, M.A., M.D.
Co-Director, Edward Via College of Osteopathic Medicine
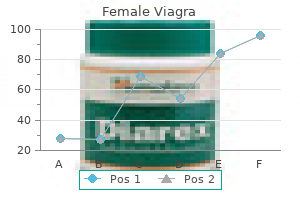
It should be remembered women's health center utexas discount female viagra 100mg with mastercard, however pregnancy 0 thru 40 wks order genuine female viagra line, that proteinuria is not always present in glomerular or nonglomerular renal disease. The use of these tests in an individual patient should be based in most cases on the relative risk of significant urinary tract pathology. Proteinuria Although healthy adults excrete 80 to 150 mg of protein in the urine daily, the qualitative detection of proteinuria in the urinalysis should raise the suspicion of underlying renal disease. Proteinuria may be the first indication of renovascular, glomerular, or tubulointerstitial renal disease, or it may represent the overflow of abnormal proteins into the urine in conditions such as multiple myeloma. Proteinuria can also occur secondary to nonrenal disorders and in response to various physiologic conditions such as strenuous exercise. The protein concentration in the urine depends on the state of hydration, but it seldom exceeds 20 mg/dL. In patients with dilute urine, however, significant proteinuria may be present at concentrations less than 20 mg/dL. Normally, urine protein is about 30% albumin, 30% serum globulins, and 40% tissue proteins, of which the major component is Tamm-Horsfall protein. This profile may be altered by conditions that affect glomerular filtration, tubular reabsorption, or excretion of urine protein. Determination of the urine protein profile by such techniques as protein electrophoresis may help determine the etiology of proteinuria. Most causes of proteinuria can be categorized into one of three categories: glomerular, tubular, or overflow. Glomerular proteinuria is the most common type of proteinuria and results from increased glomerular capillary permeability to protein, especially albumin. Glomerular proteinuria occurs in any of the primary glomerular diseases such as IgA nephropathy or in glomerulopathy associated with systemic illness such as diabetes mellitus. Glomerular disease should be suspected when the 24-hour urine protein excretion exceeds 1 g and is almost certain to exist when the total protein excretion exceeds 3 g. Tubular proteinuria results from failure to reabsorb normally filtered proteins of low molecular weight such as immunoglobulins. In tubular proteinuria, the 24-hour urine protein loss seldom exceeds 2 to 3 g and the excreted proteins are of low molecular weight rather than albumin. Disorders that lead to tubular proteinuria are commonly associated with other defects of proximal tubular function such as glucosuria, aminoaciduria, phosphaturia, and uricosuria (Fanconi syndrome). Overflow proteinuria occurs in the absence of any underlying renal disease and is due to an increased plasma concentration of abnormal immunoglobulins and other low-molecular-weight proteins. The increased serum levels of abnormal proteins result in excess glomerular filtration that exceeds tubular reabsorptive capacity. The most common cause of overflow proteinuria is multiple myeloma, in which large amounts of immunoglobulin light chains are produced and appear in the urine (Bence Jones protein). Qualitative detection of abnormal proteinuria is most easily accomplished with a dipstick impregnated with tetrabromophenol blue dye. The color of the dye changes in response to a pH shift related to the protein content of the urine, mainly albumin, leading to the development of a blue color. Because the background of the dipstick is yellow, various shades of green will develop, and the darker the green, the greater the concentration of protein in the urine. Evaluation of essential hematuria (circular erythrocytes, no erythrocyte casts, no significantproteinuria). Nephrotic range proteinuria in excess of 1 g/24 hr, however, is seldom missed on qualitative screening. Precipitation of urinary proteins with strong acids such as 3% sulfosalicylic acid will detect proteinuria at concentrations as low as 15 mg/dL and is more sensitive at detecting other proteins and albumin. Patients whose urine is negative on dipstick but strongly positive with sulfosalicylic acid should be suspected of having multiple myeloma, and the urine should be tested further for Bence Jones protein. If qualitative testing reveals proteinuria, this should be quantitated with a 24-hour urinary collection.
The procedure for using the antidote kit is as follows: Step 1: Amyl nitrite inhalant perles is only a temporizing measure (forms only 2% to 5% methemoglobin) and it can be omitted if venous access is established pregnancy resource center grand rapids order on line female viagra. Step 2: Sodium nitrite ampule is indicated for cyanide exposures breast cancer symptoms buy 100mg female viagra amex, except for cases of residential fires, smoke inhalation, and nitroprusside or acetonitrile poisonings. It is administered intravenously to produce methemoglobin of 20% to 30% at 35 to 70 minutes after administration. Step 3: Sodium thiosulfate is useful alone in cases of smoke inhalation, nitroprusside toxicity, and acetonitrile toxicity and should not be used at all in cases of hydrogen sulfide poisoning. If cyanide symptoms recur, further treatment with nitrites or the perles is controversial. Some authorities suggest repeating the antidotes in 30 minutes at half of the initial dose, but others do not advise this for lack of efficacy. One hour after antidotes are administered, the methemoglobin level should be obtained and should not exceed 20%. Gastrointestinal decontamination of oral ingestion by activated charcoal is recommended but is not very effective because of the rapidity of absorption. Acidosis should be treated with sodium bicarbonate if it does not rapidly resolve with therapy. Other antidotes include hydroxocobalamin (vitamin B12a) (Cyanokit), which has proven effective when given immediately after exposure in large doses of 4 g (50 mg/kg) or 50 times the amount of cyanide exposure with 8 g of sodium thiosulfate. Patients requiring antidote administration should be admitted to the intensive care unit. Digitalis Cardiac glycosides are found in cardiac medications, common plants, and the skin of the Bufo toad. Pacemaker cells are inhibited, and the refractory period is prolonged, leading to atrioventricular blocks. Management If the cyanide was inhaled, the patient must be removed from the contaminated atmosphere. Immediate administration of 100% oxygen is called for and oxygen should be continued during and after the Toxic Dose Digoxin total digitalizing dose, the dose required to achieve therapeutic blood levels of 0. Serious and fatal overdoses are more than 4 mg in a child and more than 10 mg in an adult. In cases of chronic or acute-on-chronic ingestions in patients with cardiac disease, more than 2 mg may produce toxicity; however, toxicity can develop within therapeutic range on chronic therapy. Patients at greatest risk of overdose include those with cardiac disease, those with electrolyte abnormalities (low potassium, low magnesium, low T4, high calcium), those with renal impairment, and those on amiodarone (Cordarone), quinidine, erythromycin, tetracycline, calcium channel blockers, and -blockers. Management A cardiology consult should be obtained and a pacemaker should be readily available. In undertaking gastrointestinal decontamination, excessive vagal stimulation should be avoided. Activated charcoal should be administered, and if a nasogastric tube is required for the activated charcoal, pretreatment with atropine (0. Problems associated with Fab therapy are mainly from withdrawal of digoxin and worsening heart failure, hypokalemia, decrease in glucose (if the patient has low glycogen stores), and allergic reactions (very rare). Digitalis administered after Fab therapy is bound and may be inactivated for 5 to 7 days. An empiric dose is 10 vials in adults and 5 vials in a child for an unknown amount ingested in a symptomatic patient with history of a digoxin overdose. For ventricular tachydysrhythmias, electrolyte disturbances should be corrected by the administration of lidocaine or phenytoin. Magnesium should be discontinued if hypotension, heart block, or decreased deep tendon reflexes are present. In cases of oral overdose, the typical onset is 30 minutes, with peak effects in 3 to 12 hours.
The medication is indicated as a first-line therapy for children with monosymptomatic nocturnal enuresis associated with nocturnal polyuria and normal bladder function menstruation 6 weeks safe female viagra 100 mg. Desmopressin is available in a sublingual lyophilisate (melt) preparation women's health magazine birth control article buy cheap female viagra line,2 as well as a tablet. The bioavailability of the lyophilisate (melt) preparation is approximately 60% greater than that of the tablet formulation. The recommended dose of desmopressin is 120 to 240 g melt and 200 to 400 g tablet. The former is usually given 30 minutes to 1 hour before bedtime, and the latter is usually given 1 hour before bedtime. Side effects are rare and include symptomatic hyponatremia with water intoxication. When desmopressin is prescribed, patients should be instructed to avoid high fluid intake in the evening. Imipramine (Tofranil), a tricyclic agent with antimuscarinic property, may be helpful in children who have not responded to desmopressin alone. Presumably, the medication decreases the amount of time spent in rapid eye movement sleep, stimulates antidiuretic hormone secretion, and relaxes the detrusor muscle. The recommended starting dose is 25 mg for children 6 to 12 years of age and 50 mg for those older than 12 years, given 1 to 2 hours before bedtime. If necessary, the dose may be increased gradually to a maximum of 50 mg in children 6 to 12 years of age and 75 mg for those older than 12 years. However, potential side effects (anxiety, depression, dizziness, headache, drowsiness, lethargy, sleep disturbance, dry mouth, anorexia, vomiting, skin rashes) and serious adverse effects (hepatotoxicity, cardiotoxicity) with overdose limit their use. Monotherapy with oxybutynin (Ditropan),1 an anticholinergic and antispasmodic agent that decreases uninhibited bladder contraction, is not effective in treating monosymptomatic nocturnal enuresis. The medication can be added, however, as a second-line drug in the treatment of children with both diurnal and nocturnal enuresis. Enuretic alarm is indicated as a first-line therapy for children with monosymptomatic nocturnal enuresis associated with a small bladder capacity or nocturnal detrusor overactivity. Randomized controlled trials have demonstrated that the enuretic alarm has greater efficacy than other forms of treatment. The enuretic alarm is triggered when a sensor in the sheets or night clothes gets wet; a bell or buzzer is thereby activated. Presumably, alarm therapy startles the child and improves arousal from sleep either by classical conditioning or avoidance conditioning. A disadvantage of alarm therapy is that it takes a couple of weeks to take effect. As such, alarms should be used for at least 6 weeks in children who do not respond before discontinuing their use. Because success depends on a cooperative, motivated child, conditioning therapy with an alarm device is generally used in children over 6 years of age. It has been shown that combination of alarm and desmopressin works better than either treatment alone. When an anatomic abnormality or defect in urinary concentration ability is present, the underlying problem may require specific dietary, pharmacologic, or surgical treatment. Combination of the enuresis alarm and desmopressin: Second line treatment for nocturnal enuresis. The comparative safety of oral versus intranasal desmopressin in the treatment of children with nocturnal enuresis. This is a normal stooling pattern so long as the infant shows no signs of distress or illness. Therefore, adequate nutrition carries special significance during this phase of life. Caregivers should always respect the choice of the mother and support her during her bonding period with her newborn infant. She may have several concerns about breast-feeding including returning to work, the logistics of pumping, or her modesty, or she may consider breast-feeding to be "antiquated. For example, some Hispanic women are concerned that when breast-feeding they might inadvertently pass on negative emotions to their newborn. Because Somalian mothers attribute special powers to Western medicine and infant formulas, they often breast-feed but supplement with formula to ensure their infant gets everything that modern medicine can offer. With proper education and support, many mothers find breast-feeding to be a more reasonable option than they first thought.

Continued smoking increases this risk menopause zits purchase generic female viagra on line, so patients should be counseled in smoking cessation breast cancer youngest age trusted 50mg female viagra. In those patients whose cancers recur and are retreated, subsequent 5-fluorouracil prophylaxis, with a single application biweekly, is used successfully to minimize further recurrences. In addition, up to 30% of patients have a synchronous adenocarcinoma of the breast, colon, rectum, or upper genital tract. To assess for invasion, the lesion should be excised via wide local excision or simple vulvectomy with at least 5 mm of the adjacent subcutaneous tissue. However, the risk of recurrence is approximately 30% whether margins are negative or positive. Thus expectant management, reserving treatment for symptomatic recurrences, is usually recommended. Most patients present with a combination of symptoms, including pruritus, discomfort, and complaints of a mass. Examination frequently reveals a suspicious lesion, which should be biopsied for diagnosis. Factors that influence dissemination include tumor size (Table 2), depth of invasion (Table 3), lymphovascular space invasion, and tumor grade. Squamous Cell Carcinomas and Adenocarcinomas Surgical management of squamous cell carcinomas and adenocarcinomas depends on the size, depth of invasion, and location of the lesion. Those without these characteristics or have palpable lymph nodes of the contralateral side require bilateral assessment. This surgical approach is associated with significant morbidity including disfigurement, wound breakdown, and problems with lymphocysts and chronic lymphedema. For patients with very large lesions or lesions in sensitive areas such as the clitoris, preoperative radiation, followed by less radical excision of residual disease, may minimize problems with the vulvar wound. Current investigations are ongoing in the use of sentinel lymph node dissections as a method of minimizing the groin morbidity without sacrificing survival. Positive vulvar margins or metastases to lymph nodes are managed with postoperative radiation. Verrucous Carcinoma Vulvar Neoplasia 1091 Verrucous carcinoma is a large exophytic tumor that resembles giant condyloma acuminatum. It is a variant of squamous carcinomas but has an excellent prognosis because of the lack of metastases. Verrucous carcinomas have a high tendency to recur and should be managed with radical local excision. Most patients have disease on the mucosal surfaces of the vulvar introitus, clitoris, and labia minora. The vulvar lesion is treated by radical excision, but management of the groins is controversial. However, given some long-term survivors with modern melanoma therapy, either lymphadenectomy or sentinel lymph node dissection, as is done for other cutaneous melanomas, appears indicated. Basal Cell Carcinoma Basal cell carcinomas typically occur in elderly white women, are commonly located on the labia majora, and have characteristics similar to basal cell carcinomas at other sites. A malignant squamous component must be ruled out because it should be managed as a squamous cell carcinoma. Malignant melanoma of the vulva treated by radical hemivulvectomy, a prospective study of the Gynecologic Oncology Group. Greenish-yellow purulent malodorous discharge Thick, white, adherent, "cottage cheese-like" discharge Bacterial vaginosis Trichomonas Vulvovaginal candidiasis >4.