FML Forte
"Purchase fml forte 5 ml visa, allergy forecast".
By: V. Kippler, M.B. B.A.O., M.B.B.Ch., Ph.D.
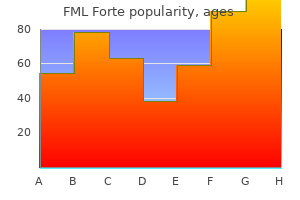
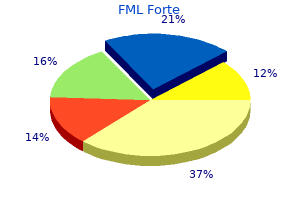
Professor, University of Arizona College of Medicine – Tucson
For instance allergy hives on legs discount fml forte 5 ml on line, some patients report dysphagia as the initial symptom of the disease allergy forecast stockton ca generic 5 ml fml forte free shipping, whereas others may never mention dysphagia. Complications from dysphagia, particularly those that threaten pulmonary function, may lead to aspiration pneumonia and death (see Chapter 6). Interestingly, the esophageal abnormalities were present even before overt manifestations of dysphagia were present. One third of the patients sampled complained of dysphagia, whereas more than 80% had objective demonstrations of its presence. Dysphagic complaints in patients receiving follow-up care in an outpatient clinic ranged between 30% and 40%. Their study showed a positive relation between dysphagia and disease severity and between dysphagia and brainstem involvement. As patients became more disabled according to a scale of disability measurement, the prevalence of dysphagia increased to 65%. In selected populations of patients with myasthenia gravis, approximately one third will be dysphagic. There are no published reports of the prevalence of dysphagia in muscular dystrophy, although there are reports of swallowing dysfunction secondary to peripheral oropharyngeal and esophageal muscle weakness in those with oculopharyngeal, Duchenne, and myotonic muscular dystrophy. Oropharyngeal dysphagia was present in 18 with dermatomyositis, and 9 with polymyositis. As with other progressive neurologic conditions, with these disorders the course and response to medical therapy may differ; therefore the presence of dysphagia is variable. Because of their predilection to involve the proximal muscle, swallowing can be affected in these disorders. Multiple disorders of pharyngeal function following videofluoroscopic swallowing studies were noted in a small group of patients with polymyositis (6), dermatomysitis (4), and inclusion body myositis. In patients with scleroderma, dysphagic complaints usually are confined to the esophagus, although secondary effects on the oral and pharyngeal stages resulting from esophageal dysmotility should be considered. They could find only estimates of prevalence ranging from 36% in the community to 73% who were inpatients. After studying those patients referred for dysphagia evaluations, Chadwick and Jolliffe69 concluded that the prevalence of those with dysphagia and concomitant mental or physical disability was 8. Observations of adults with Down syndrome living in a residential facility who were eating a regular diet revealed that 56. Those with significant neurologic delay or tracheostomy were more likely to be at risk for dysphagia. Few prevalence data have been recorded on patients with mental illness who may show signs of dysphagia. Noting this omission, Aldridge and Taylor72 completed a systematic review in an attempt to document prevalence and treatment interventions. Ten studies met the inclusion criteria documenting those with dysphagia or those who expired from choking asphyxiation. Adults with mental illness in one study were 43 times more likely to die from organic mental illness compared with the general population. None of the studies provided data on treatment intervention or outcomes (see Clinical Corner 1-3). Phagophobia, or the fear of swallowing, may be associated with psychogenic etiologic factors such as panic disorders, posttraumatic stress disorder, social phobia, or obsessive compulsive disorders. Those with phagophobia usually describe their problem as the sensation that they are unable to swallow in the absence of any documented sensory or motor abnormality. Most had serious methodologic flaws with low levels of evidence that made it too difficult to establish reliable prevalence statistics. As his condition improved and before he was allowed to eat orally, a request for a swallowing evaluation was made because it was noticed he was not swallowing his secretions well. The evaluation of swallowing revealed normal strength of the swallowing musculature; however, he was disoriented and could not maintain his alertness level for more than 30 seconds. Because of his poor mental status and alertness level, he was not allowed to eat and was considered to be at risk for dysphagia. When eating, it was noted he would take excessive time to finish, with intermittent choking episodes. The speech pathologist who evaluated him for signs and symptoms of dysphagia found that the oropharyngeal swallowing musculature was intact. As she watched the patient eat, she noted a rapid feeding rate with inappropriate bite sizes.
Because at her age and in her situation these social functions were central to her life and her well-being allergy oil blend generic 5ml fml forte fast delivery, this form of apraxia had a significant functional impact on her life allergy dizziness generic fml forte 5ml with amex. The family was instructed to prepare meals that could be eaten with a single utensil. Also, it is important to take into consideration the progressive, deteriorating nature of dementia. Although the mealtime adjustment of a single utensil was effective in the short term, as this disease progressed, this patient would require additional strategies to ensure adequate nutrition and hydration. In this respect, her treatment plan must contain periodic and regular monitoring of the success of any adaptation used to maintain oral food and liquid intake and the nutritional consequences of that intake (see Video 3-3 on the accompanying Evolve website). Martino R, Foley N, Bhogal S, et al: Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Harraf F, Ward K, Man W, et al: Transcranial magnetic stimulation study of expiratory muscle weakness in acute ischemic stroke. Ali K, Cheek E, Sills S, et al: Day-night differences in oxygen saturation and the frequency of desaturations in the first 24 hours in patients with acute stroke. Leibovitz A, Dan M, Zinger J, et al: Pseudomonas aeruginosa and the oropharyngeal ecosystem of tube-fed patients. Brogan E, Langdon C, Brookes K, et al: Respiratory infections in acute stoke: nasogastric tubes and immobility are stronger predictors than dysphagia. Axelsson K, Asplund K, Norberg A, et al: Nutritional status in patients with acute stroke. Davalos A, Ricart W, Gonzalez-Huix F, et al: Effect of malnutrition after acute stroke on clinical outcome. Neumann S, Bartolome G, Buchholz D, et al: Swallowing therapy of neurologic patients: correlation of outcome with pretreatment variables and therapeutic methods. Foley N, Teasell R, Salter K, et al: Dysphagia treatment post stroke: a systematic review or randomized controlled trials. Chouinard J, Lavigne E, Villeneuve C: Weight loss, dysphagia, and outcome in advanced dementia. Rothan-Tondeur M, Meaume S, Girard L, et al: Risk factors for nosocomial pneumonia in a geriatric hospital: a control-case onecenter study. Volicer L: Goals of care in advanced dementia: quality of life, dignity, and comfort. American Geriatrics Society Ethics Committee and Clinical Practice and Models of Care Committee: American geriatrics society feeding tubes in advanced dementia position statement. Pelletier C: What do certified nurse assistants actually know about dysphagia and feeding nursing home residents Monteleoni C, Clark E: Using rapid-cycle quality improvement methodology to reduce feeding tubes in patients with advanced dementia: before and after study. Mandaville A, Ray A, Robertson H, et al: A retrospective review of swallow dysfunction in patients with severe traumatic brain injury. Mu L, Sobotka S, Chen J, et al: Parkinson disease affects peripheral sensory nerves in the pharynx. Pitts T, Bolser D, Rosenbek J, et al: Impact of expiratory muscle strength training on voluntary cough and swallow function in Parkinson disease. Lan Y, Xu G, Dou Z, et al: the correlation between manometric and videofluoroscopic measurements of the swallowing function in brainstem stroke patients with dysphagia. Suzuki M, Asada Y, Ito J, et al: Activation of cerebellum and basal ganglia on volitional swallowing detected by functional magnetic resonance imaging. Magnus T, Beck M, Giess R, et al: Disease progression in amyotrophic lateral sclerosis: predictors of survival. Kawai S, Tsukuda M, Mochimatsu I, et al: A study of the early stage of dysphagia in amyotrophic lateral sclerosis. Ruoppolo G, Schettino I, Frasca V, et al: Dysphagia in amyotrophic lateral sclerosis: prevalence and clinical findings. Easterling C, Antinoja J, Cashin S, et al: Changes in tongue pressure, pulmonary function, and salivary flow in patients with amyotrophic lateral sclerosis.
Hynes J allergy kit for dogs buy fml forte 5ml mastercard, Nadanaciva S allergy medicine good for allergies to cats buy fml forte pills in toronto, Swiss R, Carey C, Kirwan S, Will Y (2013) A highthroughput dual parameter assay for assessing drug induced mitochondrial dysfunction provides additional predic tivity over two established mitochondrial toxicity assays. Risk factors for development of cholestatic druginduced liver injury: inhibition of hepatic basolateral bile acid transporters multidrug resistanceassoci ated proteins 3 and 4. Kurumiya Y, Nagino M, Nozawa K, Kamiya J, Uesaka K, Sano T, Yoshida S, Nimura Y (2003) Biliary bile acid concentration is a simple and reliable indicator for liver function after hepatobili ary resection for biliary cancer. Labbe G, Pessayre D, Fromenty B (2008) Druginduced liver injury through mitochondrial dysfunction: mechanisms and detection during preclinical safety studies. Lammert C, Einarsson S, Saha C, Niklasson A, Bjornsson E, Chalasani N (2008) Relationship between daily dose of oral medications and idiosyncratic druginduced liver injury: search for signals. Lammert C, Bjornsson E, Niklasson A, Chalasani N (2010) Oral medications with significant hepatic metabolism at higher risk for hepatic adverse events. Laverty H, Benson C, Cartwright E, Cross M, Garland C, Hammond T, Holloway C, McMahon N, Milligan J, Park B, Pirmohamed M, Pollard C, Radford J, Roome N, Sager P, Singh S, Suter T, Suter W, Trafford A, Volders P, Wallis R, Weaver R, York M, Valentin J (2011). Lu S, Jessen B, Strock C, Will Y (2012) the contribution of physi cochemical properties to multiple in vitro cytotoxicity end points. Massart J, Begriche K, Buron N, Porceddu M, BorgneSanchez A, Fromenty B (2013) Druginduced inhibition of mitochondrial fatty acid oxidation and steatosis. Maximos M, Bril F, Portillo Sanchez P, Lomonaco R, Orsak B, Biernacki D, Suman A, Weber M, Cusi K (2015) the role of liver fat and insulin resistance as determinants of plasma amino transferase elevation in nonalcoholic fatty liver disease. Nakayama S, Atsumi R, Takakusa H, Kobayashi Y, Kurihara A, Nagai Y, Nakai D, Okazaki O (2009) A zone classification system for risk assessment of idiosyncratic drug toxicity using daily dose and covalent binding. Olson H, Betton G, Robinson D, Thomas K, Monro A, Kolaja G, Lilly P, Sanders J, Sipes G, Bracken W, Dorato M, Van Deun K, Smith P, Berger B, Heller A (2000) Concordance of the toxicity of pharmaceuticals in humans and in animals. Porceddu M, Buron N, Roussel C, Labbe G, Fromenty B, Borgne Sanchez A (2012) Prediction of liver injury induced by chemi cals in human with a multiparametric assay on isolated mouse liver mitochondria. Opposite effects of piogli tazone and rosiglitazone on mitochondrial respiration in skeletal muscle of patients with type 2 diabetes. Regev A (2013) How to avoid being surprised by hepatotoxicity at the final stages of drug development and approval. Regev A (2014) Druginduced liver injury and drug development: industry perspective. Druginduced perturbations of the bile acid pool, chole stasis, and hepatotoxicity: mechanistic considerations beyond the direct inhibition of the bile salt export pump. Roth A, Singer T (2014) the application of 3D cell models to support drug safety assessment: opportunities & challenges. Sakuratani Y, Sato S, Nishikawa S, Yamada J, Maekawa A, Hayashi M (2008) Category analysis of the substituted anilines studied in a 28day repeatdose toxicity test conducted on rats: correla tion between toxicity and chemical structure. SimonHettich B, Rothfuss A, StegerHartmann T (2006) Use of computerassisted prediction of toxic effects of chemical sub stances. Susukida T, Sekine S, Ogimura E, Aoki S, Oizumi K, Horie T, Ito K (2015) Basal efflux of bile acids contributes to druginduced bile aciddependent hepatocyte toxicity in rat sandwichcul tured hepatocytes. Wang W, Liu X, Gelinas D, Ciruna B, Sun Y (2007) A fully automated robotic system for microinjection of zebrafish embryos. Will Y, Dykens J (2014) Mitochondrial toxicity assessment in industrya decade of technology development and insight. Willmann S, Lippert J, Schmitt W (2005) From physicochemistry to absorption and distribution: predictive mechanistic modelling and computational tools. Yu K, Geng X, Chen M, Zhang J, Wang B, Ilic K, Tong W (2014) High daily dose and being a substrate of cytochrome P450 enzymes are two important predictors of druginduced liver injury. The conclusions of these studies were not always systematically connected with the outcome of toxicology studies, and these two assessments were often disjointed. Among pharmacological tests required on respiratory, gastrointestinal, renal, central and peripheral nervous systems, etc. In contrast to the Japanese guidelines of 1995, it was preferable to use unanesthetized, unrestrained, conscious telemetered animals.
To further define the disorder allergy medicine coughing fml forte 5 ml low cost, these specialists often need the services of a radiologist allergy medicine in china discount fml forte 5ml otc. Those whose swallowing disorder may be of esophageal origin may require the services of a gastroenterologist. If the swallowing disorder is related to an acute respiratory condition, a patient may be under the care of a pulmonologist, pulmonary physical therapist, and respiratory therapist. If the swallowing disorder is related more to the process of feeding, an occupational therapist frequently is involved. If the swallowing disorder results in compromise to the nutritional system, a dietitian is consulted. In short, patients with swallowing disorders require the attention of many specialists who must work in concert to achieve swallowing safety and nutritional stability. The prominence of individual roles at any given time depends on the patient presentation. Some medical centers have designated swallowing teams and swallowing team leaders. For instance, some gastroenterologists diagnose and treat swallowing problems that involve the esophagus, but disorders of the esophagus are not their special interest. For instance, few radiologists have a specific interest in patients who report dysphagia. The result of this variance in interest and focus is that not all swallowing disorder teams are the same, and in some cases not all potential members are represented. These include an outline of the knowledge and skills needed to treat oropharyngeal dysphagia and the need to understand the esophageal components of swallowing to make appropriate medical referrals. Treating patients with dysphagia labeled one as borderline heretic with threats of a breach of ethics. George Larsen, also working in a medical setting with adults, began to develop treatments specific to patients with neurogenic swallowing disorders. Because so many of his patients with speech and language disorders had accompanying swallowing dysfunction, he began to search the literature for relevant treatment approaches. He discovered a literature full of descriptions of how a person swallows but no mention of how to treat the impairment. Using his background in neurology and physiology, he began to develop treatment approaches and reported them in the literature. He wrote about appropriate postures85 and the need for some patients to bring the swallowing sequence under volitional control. Larsen approached the patient with a probe tip wrapped in gauze, dipped in saline solution, and attached to a primitive facial nerve stimulator. As he applied the electric current to the thyroid notch, a swallow was initiated and the patient continued to swallow without the assistance of the stimulation. Our collective elation that "treatment" could be so easy was quickly dampened when Dr. Larsen warned it could be dangerous to use such a technique with every patient because it could trigger laryngospasm and death. We learned two things that day: not all treatments are for every patient, and some treatments carry accompanying risk. Otolaryngologist the otolaryngologist is skilled in the evaluation of the upper digestive tract. In particular, the use of endoscopy by otolaryngologists for direct visualization of the structures of the nasopharynx, oropharynx, pharynx, and larynx adds information relative to the structural, sensory, and motor aspects of the pharyngeal stage of swallowing. In patients with head and neck cancer who require surgery, otolaryngologists provide surgical and postsurgical management. In this regard, they must be sensitive not only to issues of cancer control, but also to the preservation of speech and swallowing functions. Because these tubes may interfere with normal swallowing, these specialists work with the dysphagia team to remove the tubes as soon as medically feasible. Gastroenterologist the gastroenterologist who participates on the swallowing disorders team usually has a special interest in the esophagus. Because primary esophageal disorders that precipitate dysphagia can have secondary effects on the pharyngeal and oral stages of swallowing, it is important to include the gastroenterologist in the evaluation of the patient who may appear to only have symptoms that relate to the oral or pharyngeal stages of swallowing (see Chapter 5). The gastroenterologist may use special sensors that measure the amount of acid content in the alimentary tract using a test called 24hour pH monitoring.
Spindle Cell Proliferation Admixed With Vascular Spaces Slit-Like Spaces Containing Red Blood Cells (Left) Monomorphic spindle cells in ill-defined fascicles and arcs intimately admixed with slit-like vascular channels containing erythrocytes are a classic feature of Kaposi sarcoma allergy medicine by prescription generic 5 ml fml forte with visa. They expand the vascular spaces of the corpus spongiosum with atrophy of the vessel walls and loss of the lumen allergy medicine starts with l generic 5ml fml forte with visa. Myointimoma: Myofibroblastic Proliferation Myointimoma: Intravascular Growth (Left) In these peripheral transition areas, there is partial filling of small vessel lumina by the lesional spindled cells with associated myxoid stroma. Residual endothelial cells and smooth muscle collarettes are common in these foci. Metastatic Adenocarcinoma to Penis Metastatic Nodules in Penis (Left) Transverse section shows extensive involvement of both corpora cavernosa as well as periurethral tissue. The papillary surface of the tumor is lined by small basaloid cells at the center and larger pink cells with koilocytic changes at the periphery. Biphasic histology, presence of squamous cell carcinoma in situ, and previous history of squamous cell carcinoma support sarcomatoid differentiation. Leiomyosarcoma and sarcomatoid carcinoma are other spindle cell malignancies that more commonly involve the penis. Leiomyosarcoma is typically positive for actin-sm and desmin; cytokeratin may be aberrantly expressed, although usually focal. Adenocarcinoma - with aberrant p63 expression, 628, 637 Gleason grading of, 629 - acinar. Corpora amylacea, 545 - in acinar adenocarcinoma, 610 Cortex, 262 Cowper gland duct cyst, urethral diverticula vs. Cystic kidney disease, localized or segmental, cystic partially differentiated nephroblastoma vs. Ectopic prostate tissue, 495 Ejaculatory duct epithelium - atypical small acinar proliferations vs. Enteric-type adenocarcinoma, 471 - involving bladder, markers in, 529 Eosinophilic amorphous secretions, in acinar adenocarcinoma, 610 Eosinophilic cystitis, 266, 270 Eosinophilic variant chromophobe renal cell carcinoma, succinate dehydrogenase complex deficiency syndrome vs. Fibromuscular stroma, renal tumors with - clear cell papillary renal cell carcinoma vs. Flat urothelial lesions, 250 - markers used in, 528 - urethral, with atypia, nephrogenic adenoma (metaplasia) of prostatic urethra vs. Glandular differentiation, invasive urothelial carcinoma with, tumors of urachus vs. Hereditary prostate cancer, 609 Heterologous osteosarcoma, sarcomatoid urothelial carcinoma, 400 High-grade acinar adenocarcinoma, with cribriform pattern, prostatic intraepithelial neoplasia vs. Invasive urothelial carcinoma, 330 - with glandular differentiation, tumors of urachus vs. Metastasis - distant, 328 germ cell tumors, 751 - in lymph node, urothelial carcinoma of renal pelvis, 512 - testicular tumors vs. Mixed architectural patterns, well-differentiated neuroendocrine tumor (carcinoid)/high-grade neuroendocrine carcinoma, 209 Mixed cell tumor, 904 Mixed epithelial and stromal tumor - renomedullary interstitial cell tumor vs.