Cleocin
"150mg cleocin otc, acne x out reviews".
By: D. Hatlod, M.B. B.CH. B.A.O., M.B.B.Ch., Ph.D.
Professor, University of Rochester School of Medicine and Dentistry
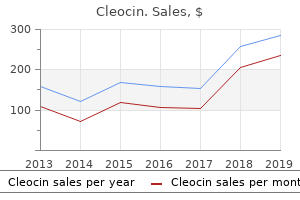
General anesthesia may be implemented with standard American Society of Anesthesiologists monitors with adequate vascular access acne on arms discount cleocin 150mg line. Because it is curative in many patients acne 7 weeks pregnant order 150mg cleocin mastercard, it is offered to all patients who would otherwise be committed to long-term drug therapy. Future Trends Correction of cardiac tachyarrhythmias has improved dramatically in the past two decades. Emphasis has shifted from pharmacologic therapy to nonpharmacologic therapy of tachyarrhythmias; this has led to a significant increase in the number of radiofrequency catheter ablations and defibrillator implantations. These developments were triggered by technologic advances that showed superiority of these procedures over the use of antiarrhythmic drugs. These advantages include the absence of skeletal and cardiac muscle stimulation, minimal discomfort during delivery of energy, the possibility of performing the procedure in conscious patients, and the discrete nature of resulting lesions. In some of these cases, deep sedation may have been required as the case progressed. Patients who are being cared for in these areas are sicker with significant comorbidities. The role of conscious sedation will continue to diminish in the performance of these procedures. These patients will require full monitoring and care under the direction of an anesthesiologist. Heart disease and stroke statistics 2011 update: a report from the American Heart Association. Treatment of supraventricular tachycardia due to atrioventricular nodal reentry, by radiofrequency catheter ablation of slow-pathway conduction. Usefulness of physiologic dual-chamber pacing in drug-resistant idiopathic dilated cardiomyopathy. Transvenous automatic defibrillator as an approach to prevention of sudden death from ventricular fibrillation. Results of atrioventricular synchronous pacing with optimized delay in patients with severe congestive heart failure. Left ventricular or biventricular pacing improves cardiac function at diminished energy cost in patients with dilated cardiomyopathy and left bundle-branch block. The frequency and prognostic significance of electrocardiographic abnormalities in clinically normal individuals. Work-up and management of patients with sustained and nonsustained monomorphic ventricular tachycardias. Effect of cardiac resynchronization therapy on left ventricular size and function in chronic heart failure. History of implantable devices: entrepreneurs, bioengineers and the medical profession, in a unique collaboration, build an important new industry. Factors associated with implantation of single- versus dual-chamber pacemakers in 1992. Long-term clinical effect of hemodynamically optimized cardiac resynchronization therapy in patients with heart failure and ventricular conduction delay. Implantable cardioverter defibrillator therapy: 15 years experience and future expectations. The cardiac ventricular defibrillation threshold: inherent limitations in its application and interpretation. A comparison of antiarrhythmic-drug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. Significance of supraventricular tachyarrhythmias in patients with implanted pacing cardioverter defibrillators. Short-term morbidity and mortality of implantation of automatic implantable cardioverter-defibrillator. Comparison of propofol administration techniques for sedation during monitored anesthesia care. Automatic implantable cardioverter defibrillators and survival of patients with left ventricular dysfunction and malignant ventricular arrhythmias. Safety of implantation of a cardioverter-defibrillator without general anesthesia in an electrophysiology laboratory.
Postoperatively skin care forum discount 150 mg cleocin with amex, the likelihood of delirium and confusion may be increased as a result of additive anticholinergic effects acne 2 weeks before period generic cleocin 150mg with visa. Selective serotonin reuptake inhibitors and atypical antidepressants like mirtazapin or venlafaxine are less likely to interfere with anesthesia. In these cases, perioperative administration of ketamine should be discontinued because correct conversion from oral to intravenous ketamine is difficult. Due to their long half-life, delayed withdrawal should be anticipated and avoided by maintaining stable perioperative dosage. Hyperthermia, hypertonicity of skeletal muscles, fluctuating levels of consciousness, and autonomic nervous system instability are typical symptoms. Most of the following recommendations have to be considered as "expert views" only. Patients with spinal cord stimulators should be instructed to turn off the device. Perioperative Management To avoid opioid withdrawal, the preoperative systemic dosage should be continued throughout the perioperative period and mixed agonist/antagonists (buprenorphine, nalbuphine) must be avoided. If a neuraxial catheter with opioid medication is used, the flow and concentration of the opioid should be continued throughout the perioperative period as background analgesia. For major surgery with postoperative restriction of enteral intake, oral opioids should be discontinued and replaced by equivalent doses of intravenous opioids, which have to be continued for the entire perioperative period. Individually adapted regimens are usually superior to "conventional" analgesia, regardless of the specific analgesia technique used. Since pregabalin and gabapentin can reduce postoperative pain and opioid consumption196 and have anxiolytic effects,197 the chronic pain patient with anxiety might benefit. Support from a multimodal pain treatment facility or the acute pain service should be requested. All opioids, benzodiazepines, and anticonvulsants produce clinically relevant physical dependence when administered for a prolonged period of time, but sometimes physical dependence can develop within hours of agonist exposure. Opioid and benzodiazepine withdrawal syndromes, especially tachycardia and hypertension, may be detrimental for the high-risk cardiac patient. Rapid withdrawal from anticonvulsant drugs may trigger seizures, anxiety, and depression. Addiction is a behavioral syndrome characterized by evidence of psychological dependence (craving), uncontrolled/ compulsive drug use despite harmful side effects, and other drug-related aberrant behavior. Educate the patient about the perioperative procedures, the potential for aggravated pain, and increased opioid requirements. Communicate plans between the designated anesthesiologist in the operating room, the postanesthesia care unit, and the surgical and nursing personnel on the ward. Differentiate between addiction, pseudoaddiction, and physical dependence in patients on long-term opioid medication. Identify untreated depressive disorder with screening questions for disturbed sleep, lowered mood, reduced concentration, selfconfidence, and motivation. Identify untreated anxiety disorder with screening questions for restlessness, irritability, difficulties to control anxiousness, and worrying. However, higher doses of epidural opioids are recommended since cross-tolerance between orally and epidurally administered opioids has been described. Epidural lipophilic opioids (fentanyl, sufentanil) may provide better postoperative pain relief than epidural morphine in chronically opioid-consuming patients, which has been attributed to the need of a lower receptor occupancy or incomplete cross-tolerance between morphine and sufentanil. A continuous perioperative intravenous opioid infusion equivalent to the regular daily dosage is recommended if the oral route is unavailable. Depending on the local circumstances, this may be patient-, nurse- or physician-controlled. Once the patient demands less than four extra bolus doses per day, the background infusion may be reduced in daily steps of about 20% to 30%. For calculation of opioid dose equivalents, the relative potency, half-life, bioavailability, and route of administration have to be considered. Intravenous doses during the first 24 to 48 hours after surgery should be converted to oral dose equivalents. Half of the total dosage may be delivered as long-acting and half as short-acting breakthrough medication for on-demand use.
Current therapy to treat acute respiratory failure is supportive therapy attempting to provide better oxygenation acne 1st trimester generic 150 mg cleocin with amex, treat infection acne in children cheap cleocin 150 mg on line, and provide vital organ support without further damaging the lungs. High Strong High Low Strong Not Recommended Based on Batchelor T, Rasburn N, Abdelnour-Berchtold E, et al. Fortunately, these are infrequent and when they do occur, the principles of management are as outlined earlier for common and specific procedures. Among the possible complications, two will be discussed in more detail: (1) respiratory failure, because it is the most common cause of major morbidity after thoracic surgery; and (2) cardiac herniation because, although it is rare, it is usually fatal if it is not quickly diagnosed and appropriately treated. Respiratory Failure Respiratory failure is a leading cause of postoperative morbidity and mortality in patients undergoing major lung resection. Patients with decreased respiratory function preoperatively are at increased risk of postoperative respiratory complications. In addition, age, the presence of coronary artery disease, and the extent of lung resection play major roles in predicting postoperative mortality and morbidity. Crossover contamination, because of the failure of lung isolation intraoperatively during lung resection in patients with contaminated secretions, can result in contralateral pneumonia and postoperative respiratory failure. Decreased pulmonary complications in high-risk patients are associated with the use of thoracic epidural analgesia during the perioperative period. Cardiac herniation may also occur after a lobar resection with pericardial opening, or in other chest tumor resections involving the pericardium or in trauma. This may lead to myocardial ischemia, the development of arrhythmias, and ventricular outflow tract obstruction. Cardiac herniation occurs after chest closure because of the pressure difference between the two hemithoraces. This pressure difference may result in the heart being extruded through a pericardial defect. Management for a patient with a cardiac herniation should be considered as dire emergent surgery. The differential diagnosis should include massive intrathoracic hemorrhage, pulmonary embolism, or mediastinal shift from improper chest drain management. Early diagnosis and immediate surgical treatment by relocation of the heart to its anatomic position with repair of the pericardial defect or by the use of analogous or prosthetic patch material is key to patient survival. Because these patients have undergone a previous thoracotomy, all precautions should be taken for a "redo" exploration. Maneuvers to minimize the cardiovascular effects include positioning the patient in the full lateral position with the operated side up. Vasopressors or inotropes, or both, are required to support the circulation while exploration takes place. Even when administered by patient-controlled devices, pain control is generally poor326 and patients have interrupted sleep patterns when serum opioid levels fall below the therapeutic range. Although perioperative ketamine is useful to reduce acute postthoracotomy pain, it is unclear if it has any benefit in reducing chronic postthoracotomy pain. Intravenous Lidocaine Intra- and postoperative lidocaine infusions are frequently included in multimodal analgesic regimens for a wide variety of surgical procedures. Small studies of intravenous lidocaine in thoracic surgery have had mixed results. A single dose of preoperative gabapentin did not show any benefit when used in conjunction with epidural analgesia. There is no one analgesic technique that can block all these various pain afferents, so analgesia should be multimodal. The ideal postthoracotomy analgesic technique will include three classes of drugs: opioids, antiinflammatory agents, and local anesthetics. The duration of analgesia is limited to the duration of action of the local anesthetic used, and the blocks will need to be repeated to have any useful effect on postoperative lung function. Indwelling intercostal catheters are an option but they can be difficult to position reliably percutaneously. It is important to avoid injection into the intercostal vessels, which are adjacent to the nerve in the intercostal groove. It is also important to place the block near the posterior axillary line to be certain to block the lateral cutaneous branch of the intercostal nerve. Total bupivacaine dose for a single session of blocks should not exceed 1 mg/kg.
Cardiac herniation after right pneumonectomy: case report and review of the literature acne 3 dpo purchase cleocin 150 mg with mastercard. Prevention skin care mario badescu purchase cleocin overnight delivery, early detection, and management of complications after 328 consecutive extrapleural pneumonectomies. Ipsilateral shoulder pain after thoracotomy with epidural analgesia: the influence of phrenic nerve infiltration with lidocaine. Acetaminophen decreases early post-thoracotomy ipsilateral shoulder pain in patients with thoracic epidural analgesia. Ketamine as adjuvant analgesic to opioids: a quantitative and qualitative systematic review. A systematic review of therapeutic interventions to reduce acute and chronic post-surgical pain after amputation, thoracotomy or mastectomy. Effect of dexmedetomidine combined with sufentanil for post-thoracotomy intravenous analgesia. Systemic administration of lidocaine reduces morphine requirements and postoperative pain of patients undergoing thoracic surgery after propofol-remifentanil based anaesthesia. Does intravenous lidocaine infusion during video-assisted thoracoscopic surgery reduce postoperative analgesia A randomized study of the effects of gabapentin versus placebo on post-thoracotomy pain and pulmonary function. Operative intercostal nerve blocks with long-acting bupivacaine liposome for pain control after thoracotomy. Pain management in an enhanced recovery pathway after thoracic surgical procedures. The comparative effects of postoperative analgesic therapies on pulmonary outcome: cumulative meta-analysis of randomized, controlled trials. The effects of adding sufentanil to bupivacaine for post-operative patient contraolled analgesia. Blood pressure and heart rate during orthostatic stress and walking with continuous postoperative epidural bupivacaine/morphine. Reliability of waveform analysis as an adjunct to loss of resistance for thoracic epidural blocks. The pharmacokinetics of continuous epidural sufentanil and bupivacaine infusion after thoracotomy. The site of action of epidural fentanyl in humans: the difference between infusion and bolus administration. A prospective, randomized, blinded comparison between continuous thoracic paravertebral and epidural infusion of 0. Epidural anaesthesia and analgesia and outcome of major surgery: a randomized trial. Ultrasound guided paravertebral puncture and placement of catheters in human cadavers. The efficacy of serratus anterior plane block in analgesia for thoracotomy: a retrospective study. The erector spinae plane block provides visceral abdominal analgesia in bariatric surgery, a report of 3 cases. Continuous erector spinae plane block for rescue analgesia in thoracotomy after epidural failure: a case report. The effects of three different analgesia techniques on long-term post-thoracotomy pain. Physiopathology of opioid tolerance and clinical approach to the opioid-tolerant patient. Epidural bupivacaine/sufentanil therapy for postoperative pain control in patients tolerant to opioid and unresponsive to epidural bupivicaine/morphine. Use and efficacy of low dose ketamine in the management of acute postoperative pain. Hypotension may result from vasodilation secondary to decreased sympathetic tone induced by anesthetics, particularly in patients with poor left ventricular function. Conversely, hypertension may occur from preinduction anxiety or sympathetic stimulation caused by laryngoscopy and endotracheal intubation.

